
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 5, September/October 2017
AFRICA
305
whereas one (8.3%) had CHD in the interventricular septum.
Eleven (91.7%) of the patients were operated on through
median sternotomy and the remaining one was operated on
via a left anterolateral thoracotomy. Ten (83.3%) patients
were operated on using cardiopulmonary bypass (CPB) under
moderate hypothermia, whereas the remaining two (16.7%) had
surgery without CPB.
During surgery, as previously described, right-sided cardiac
hydatid cysts deserve special attention, Our technique is that, while
performing the cannulation, initially a single cannula is inserted
into the superior vena cava, and after clamping the pulmonary
artery with the aorta, the inferior vena cava cannula is inserted in
order to avoid iatrogenic HC embolisation.
3
There are no special
precautions regarding left-sided CHCs in terms of cannulation.
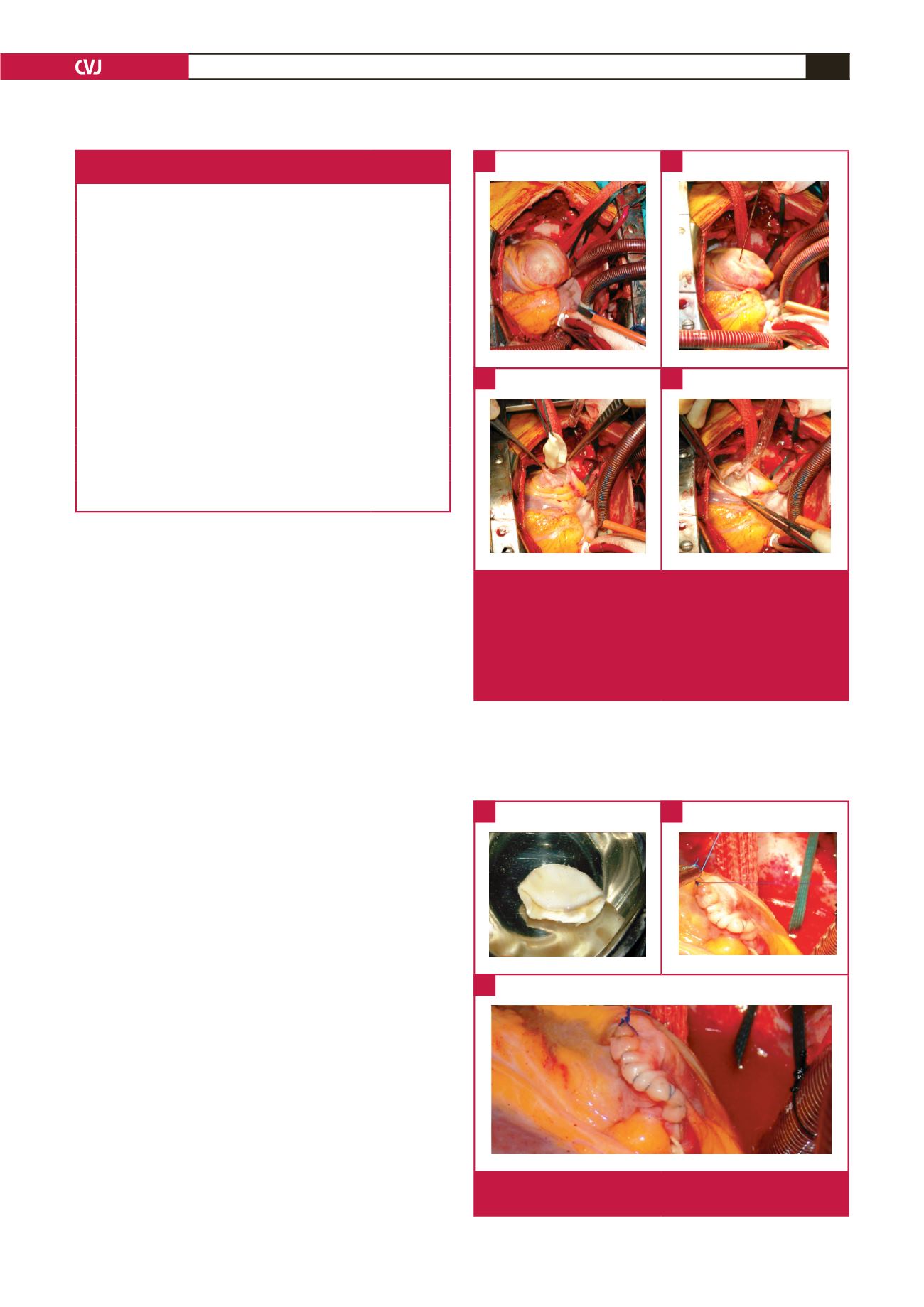
After cannulation, the surgical procedure was standard. First
the cyst was punctured with a wide aspiration needle connected
to the suction device, and after aspiration, without removing
the needle, 10% hypertonic saline was injected into the cystic
cavity for sterilisation (Fig. 1). The endocyst and the remaining
daughter cysts were then removed after gently opening the
cystic cavity. Finally, the residual cavity was closed either with
continuous or multiple interrupted prolene sutures (Fig. 2).
In our series, one of the patients, a 58-year-old male, had
CHD in the interventricular septum (Fig. 3). The patient
had interventricular cystectomy and capitonnage surgery using
standard CPB techniques under moderate hypothermia. The
patient also had a bypass to the second branch of the circumflex
(OM2) artery using a radial artery graft. All the resected material
was sent to the Pathology Department and reports indicated
either intact or degenerated HC.
There was no surgical mortality in our series. Our patients
had neither cardiac rhythm disturbances nor positive inotropic
support postoperatively. Mean intensive care unit stay was two
days (range between one and three days) after the operation, and
seven days (ranging between five and nine days) to discharge from
hospital. All patients were followed up with echocardiography. In
the first week, the results showed no worsening of left ventricular
ejection fraction, compared with pre-operative results.
All patients were discharged with either mebendazole (in six
cases) or albendazole (400 mg twice a day) treatment for six
months and all patients, except one, who was operated on one year
Table 1. Demographic data of the patients operated on
due to cardiac hydatid disease (
n
= 12)
Age (years), mean (range)
42.6 (12–65)
Gender,
n
(%)
Male
6 (50)
Female
6 (50)
Location of hydatid cyst,
n
(%)
Right sided
5 (41.7)
Right atrium
2 (16.7)
Right ventricle
2 (16.7)
RVOT
1 (8.3)
Left sided
6 (50)
Left ventricle
5 (41.7)
Left atrium
1 (8.3)
Interventricular septum
1 (8.3)
Surgical procedure: cystectomy and capitonnage,
n
(%)
Median sternotomy with CPB
10 (83.4)
Median sternotomy without CPB
1 (8.3)
Left AL thoracotomy without CPB
1 (8.3)
n
, number; RVOT, right ventricular outflow tract; AL, anterolateral; CPB,
cardiopulmonary bypass.
Fig. 1.
Surgical procedures of cardiac hydatic cystectomy.
A. Cardiac hydatid cyst located on the posterior left
ventricular wall. B. An aspiration needle inserted into
the cyst and 10% hypertonic saline injected into the
cystic cavity for sterilisation. C. Removal of the germi-
native membrane. D. Aspiration of the contents of the
cystic cavity.
A
C
B
D
Fig. 2.
A. Intact germinative membrane. B, C. Closure of the
cystic cavity.
A
C
B

















