
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
293
suspected unrelated foetal anomalies and a third case of a
complex foetal anomaly probably attributable to warfarin.
Only 20 pregnancies (69%) had a normal neonatal outcome.
The women in this cohort had lengthy hospitalisations, with 20
patients (69%) requiring more than 30 days in hospital and 15
(52%) requiring three or more admissions.
Themortality rate (6.9%) in our cohort compares unfavourably
with similar local cohorts
9,13,15
and with a large meta-analysis
showing a 2.9% rate,
2
but favourably with UKOSS, a recent
United Kingdom population-based study.
16
Both mortalities
occurred postpartum after discharge and in patients with double
valve replacements, which have been associated with worse
maternal outcomes.
16
Inducing an anticoagulated state opposes the pro-thrombotic
milieu of normal pregnancy.
17
Obstetric haemorrhage is known
to be a major contributor to maternal deaths.
18
Haemorrhage
rates were significantly high with 21% of patients having major
haemorrhagic complications. This rate is comparable with other
cohorts of women with mechanical prosthetic heart valves.
5,16
Another study
15
reported post-partum haemorrhage in only 5.8%
of patients. These variable rates may reflect differing practice in
the timing of anticoagulation reintroduction.
The anticoagulation protocol used prescribes heparin rather
than warfarin from 36 weeks’ gestation, allowing rapid reversal
of anticoagulation if required during delivery. Delivery takes
place during an anticoagulation-free ‘window’ to minimise risk of
post-partum haemorrhage. There is a need to identify the optimal
duration of this ‘window’ to balance the risks of haemorrhage
and thrombosis. Heparin is usually reinstated six hours after
delivery unless there is clinical concern of haemorrhage.
Of the 19 pregnancies delivered after viability, and
consistent with other literature,
19-21
post-operative haemorrhage
(3/9 caesarean sections, 33%) was more frequent than major
haemorrhage post-vaginal delivery (1/10 normal vaginal
deliveries, 10%), indicating that a longer anticoagulation window
may be appropriate after operative delivery. The data suggest
that caesarean sections should be performed only when clearly
indicated, with meticulous haemostasis, and in anticipation of
possible haemorrhage.
Despite the risk of major bleeding, neither death occurred as
a direct result of bleeding. However, cases of major haemorrhage
would have resulted in deaths had resuscitation, including
transfusion not been available.
Only one patient had a suspected thrombo-embolic event.
Two further patients had ischaemic strokes in the setting of HIV
positivity.
Protocols used called for intravenous unfractionated heparin
from six to 12 weeks’ gestation and peripartum, according
to relevant guidelines.
14
However, more recent guidelines
22
recommend subcutaneous low-molecular-weight heparin
(LMWH) (enoxaparin, Clexane) in preference to unfractionated
heparin (UFH), dose adjusted according to peak anti-Xa levels.
LMWH has more predictable pharmacokinetics and less risk
of allergic reactions, heparin-induced thrombocytopenia and
osteoporosis compared to UFH.
22,23
However, there is concern
that the use of subcutaneous UFHmay lead to unacceptably high
rates of treatment failure and valve thrombosis.
24
Consequently,
intravenous UFH is generally recommended and may remain the
only alternative to warfarin where access to anti-Xa monitoring
is limited, such as in our setting.
Intravenous heparin infusions are, however, resource intensive,
requiring frequent monitoring and prolonged hospitalisation.
The single suspected thrombotic event occurred in a patient
receiving UFH while in a sub-therapeutic range. However, even
ideal anticoagulation can lead to treatment failure.
In general, heparin use avoids the pregnancy loss and
embryopathy associated with warfarin but carries a higher risk
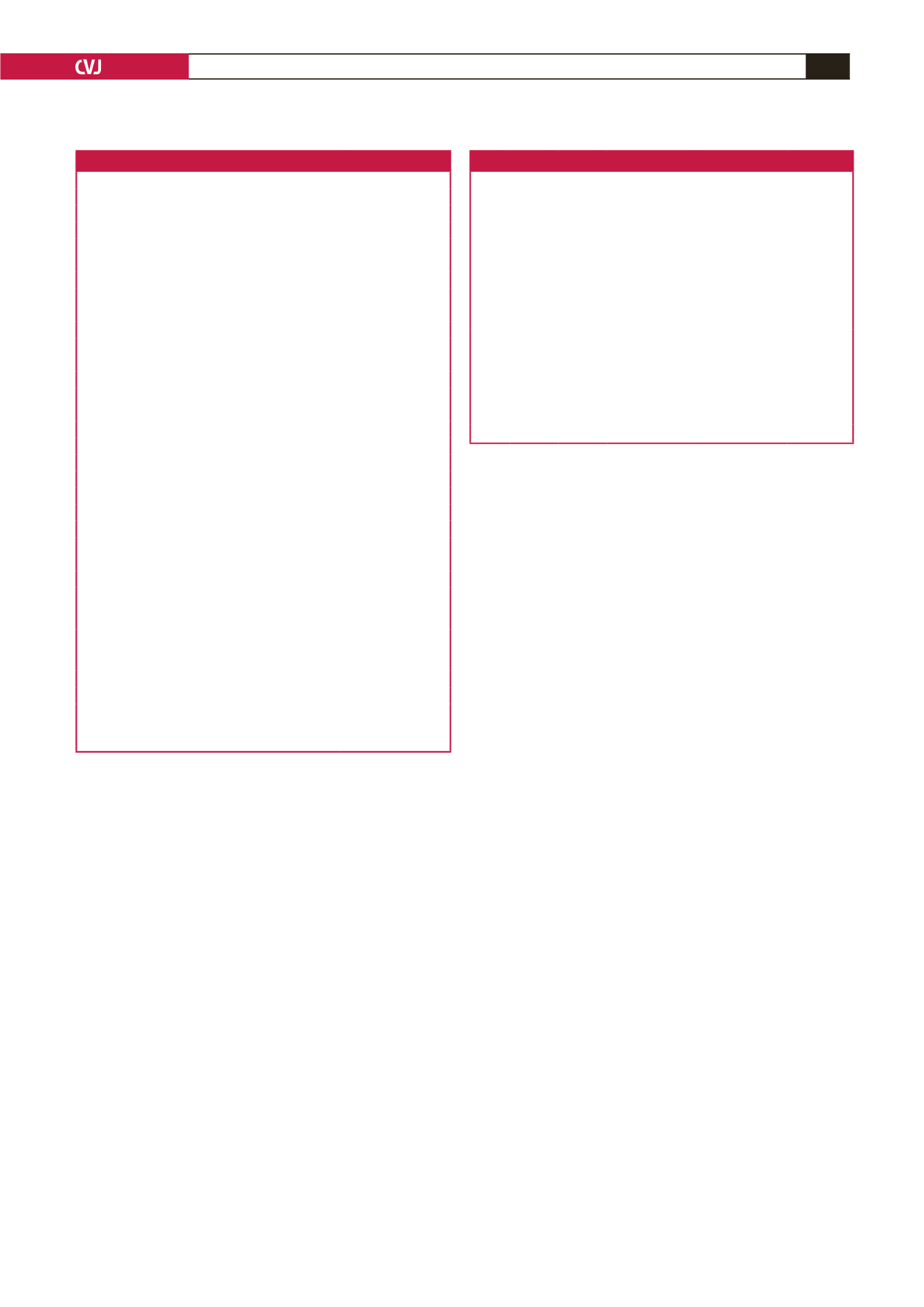
Table 5. Maternal and foetal outcomes
Outcomes
Number (%)
Maternal outcomes
NYHA FC (
n
=
13)
I/II
12
III
1
Deaths
2
Delivery
Vaginal
19 (66)
Caesarean
9 (31)
Hysterotomy
1 (3)
Reasons for surgical delivery
Foetal distress
3
Previous caesarian section
2
SROM
2
Other
3
Bleeding complications
Major bleeding
7 (24)
Blood transfusion
8 (28)
Thrombotic complications
4 (14)
Arrhythmias
11 (38)
Time in hospital
Hospital stay (days)
41
±
28
Admissions
3
±
1.8
Foetal outcomes
Healthy
19 (66)
Birth weight (g) (
n
=
19)
<
2 kg: 2
2–2.5 kg: 4
2.5–4 kg: 13
Apgar score at 5 min (
n
=
18)
Apgars 9–10: 17
Apgars 7: 1
Born before arrival: 1
ENND
1 (3)
Pregnancy loss
6 (21)
Termination
3 (10)
NYHA FC: New York Heart Association functional class, SROM: spontaneous
rupture of membranes, ENND: early neonatal death.
Table 6. Congenital abnormalities including warfarin embryopathy
Patient
no
Maternal
age
GA at 1st
antenatal
visit
Parity
Antico-
agulant
and dose Sonography
Foetal
outcomes
1
25
24
1
Warfarin,
5 mg
Polyhydramnios,
abnormal facies,
close-set eyes,
absent nose, low-
set ears, bossed
forehead, abnormal
ventricles, short
spine, fat puffy
hands and feet
ENND
2
29
17’5
2
Warfarin
5 mg in
T1 then
defaulted
Dandy–Walker
malformation
Termination
at 19 weeks
3
38
19’1
4
Warfarin
7.5 mg
daily
Echogenic bowel
Termination
at 22 weeks
GA: gestational age, ENND: early neonatal death, T1: first trimester.

















