
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
299
response of neutrophils and monocytes was similar although the
magnitude of NADPH oxidase activity was significantly higher
in neutrophils than in monocytes of patients with ARF.
18
In recent years, there has been a focus on WBC subtypes,
such as neutrophils, lymphocytes, and NLR as predictors
of cardiovascular risk. Many studies have shown that high
ratios are associated with increased inflammation in various
cardiovascular diseases. Öztürk
et al
. reported that higher
NLR was associated with spontaneous echocardiographic
contrast in rheumatic mitral valve stenosis.
19
Increased
neutrophil count was found to be associated with infarct size
and adverse angiographic outcomes in patients with myocardial
infarction,
6
while low lymphocyte count was related to adverse
outcomes in patients with myocardial infarction and chronic
heart failure.
20
Akboga
et al
. evaluated adult patients with rheumatic mitral
valve stenosis (RMS) and found median NLRs to be significantly
higher in patients with RMS compared with the control group.
Moreover, they also showed NLRs to increase with the severity
of mitral stenosis.
21
Baysal
et al
. revealed that high levels of
NLR were an independent predictor of severe RMS.
22
In a
recent study, it was reported that patients with severe RMS had
significantly higher NLRs than those with mild-to-moderate
RMS.
23
In addition, higher NLRs were associated with an
increased risk of long-term mortality in patients admitted with
acute decompensated heart failure.
24
In our study, we found that there was a significant positive
correlation between CRP, ESR and NLR in ARC, indicating
that NLR was associated with inflammation in this group of
patients. Kucuk
et al.
demonstrated a strong association of CRP
and ESR levels in children with ARC.
17
Similarly, Ozdemir
et al.
showed higher CRP and ESR levels in ARF.
25
The NLR may be the more preferable marker owing to three
factors. First, although some conditions such as exercise and
dehydration may increase the absolute number of neutrophils
and lymphocytes, NLR is less commonly affected.
26
Second,
NLR is calculated from the counts of products of two different
but complementary immune pathways.
6
Third, the reason for
the increased NLR was probably increased apoptosis of the
lymphocytes, associated with the increased inflammatory status
in ARF.
We also discovered increasing platelet counts and decreasing
MPV values in patients with ARC, which reflect the inverse
relationship between changes in platelet count and size. The
mechanism of increase in platelet volume is thought to be
that inflammatory cytokines stimulate the production of large,
reactive platelets, which have a shorter life span.
27
Sert
et al
. showed lower MPV levels in ARF patients.
14
They
speculated that lower MPV values during ARF may be related to
the effect of interleukin 6 (IL-6). In a previously reported study,
administration of IL-6 was shown to cause an increase in platelet
number as well as a decrease in MPV values.
28
Previous studies
showed that serum IL-6 levels were significantly elevated during
attacks of ARF.
29
Regarding the effect of IL-6 on thrombocytes,
low MPV values during ARF may be related to the effect of
IL-6. Similarly, in a prospective study, MPV values significantly
decreased together with CRP and IL-6 values and platelet counts
in response to two-year anti-rheumatic treatment, questioning
the inverse correlation between MPV and thrombocytosis.
30
Since 2015, there have been changes in the diagnosis of ARF
due to the revised Jones criteria. Changing the criteria may have
led to an increase in our patient numbers. However, at least one
extra major criterion or at least two minor criteria were definitely
identified besides clinical carditis in the patient group prior to
2015. Therefore none of the ARC patients were excluded from
the study.
Although conducted with a relatively large ARC patient
cohort, the retrospective design represents this study’s main
limitation. Also we could not find follow-up full blood count
values for the majority of patients due to their lack of adherence.
Therefore the study was conducted using pre-treatment blood
values.
Conclusion
NLR and MPV are simple, rapid and easily accessible
inflammatory markers that could be prognostic parameters
associated with the severity of valvular involvement in ARC.
However, prospective studies with larger numbers of patients are
needed to evaluate the role of NLR and MPV values in ARC.
References
1.
Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden
of group A streptococcal diseases.
Lancet Infect Dis
2005;
5
(11):
685–694.
2.
Sika-Paotonu D, Beaton A, Raghu A, Steer A, Carapetis J. Acute
rheumatic fever and rheumatic heart disease. In: Ferretti JJ, Stevens
DL, Fischetti VA, eds.
Streptococcus pyogenes
: Basic Biology to
Clinical Manifestations [Internet]. Oklahoma City (OK): University of
Oklahoma Health Sciences Center; 2016–2017 Mar 10 [updated 2017
Apr 3].
3.
Cunningham MW. Pathogenesis of group A streptococcal infections.
Clin Microbiol Rev
2000;
13
(3): 470–511.
4.
Guilherme L, Kalil J, Cunningham M. Molecular mimicry in the auto-
immune pathogenesis of rheumatic heart disease.
Autoimmunity
2006;
39
(1): 31–39.
5.
Zahorec R. Ratio of neutrophil to lymphocyte counts-rapid and
simple parameter of systemic inflammation and stress in critically ill.
Bratislavske Lekarske Listy
2001;
102
(1): 5–14.
6.
Azab B, Zaher M, Weiserbs KF, Torbey E, Lacossiere K, Gaddam S,
et
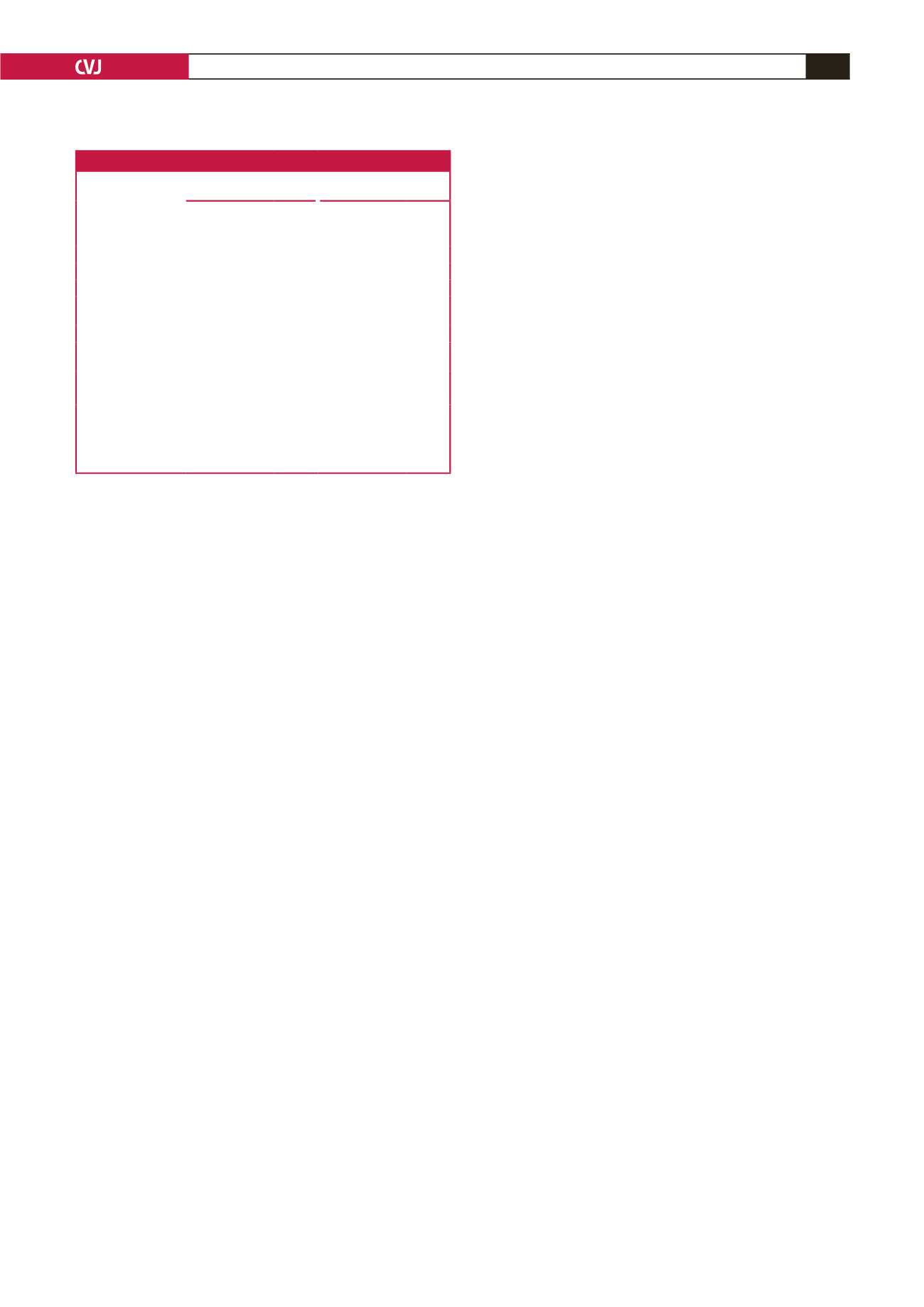
Table 2. Independent predictors of severity of valve regurgitation
Independent variables
Univariate logistic
regression
Multiple logistic
regression
OR (95% CI)
p
-value OR (95% CI)
p
-value
WBC count
(×10
3
cells/mm
3
)
0.79 (0.53–2.86)
0.034
Haemoglobin (g/dl)
1.53 (1.26–1.87)
0.042
ESR (mm/h)
0.38 (0.21–0.76)
0.50
CRP (mg/l)
0.92 (0.88–0.97)
0.22
Platelet count
(× 10
3
cells/mm
3
)
0.26 (0.18–0.52)
0.035
MPV (fl)
0.44 (0.24–0.94)
<
0.001 0.78 (0.72–0.98)
0.008
Neutrophil count
(× 10
3
cells/mm
3
)
0.85 (0.54–1.89)
0.042
NLR
0.42 (0.27–0.66)
<
0.001 0.51 (0.32–0.68)
0.006
MCV
0.36 (0.26–0.64)
0.024
Dependent variable: severe valve regurgitation cases with or without two-valve
regurgitation (
n
=
38).
OR: odds ratio, CI: confidence interval, WBC: white blood cell, ESR: erythro-
cyte sedimentation rate, CRP: C-reactive protein, MPV: mean platelet volume,
NLR: neutrophil-to-lymphocyte ratio, MCV: mean corpuscular volume (fl).

















