
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 6, November/December 2019
334
AFRICA
The 2018 European Society of Cardiology (ESC) and the
European Association for Cardiothoracic Surgery (EACTS)
published guidelines on myocardial revascularisation. They
recommended revascularisation in patients with stable angina
or silent ischaemia with a large area of ischaemia, defined as
ischaemia exceeding 10% of the left ventricular myocardium
as detected by functional testing, as a class I recommendation,
level of evidence B.
11
In these guidelines, the recommendation to
revascularise based on viability imaging is not stated.
In our study, more than half of the patients referred for
viability imaging had potentially reversible myocardial contractile
dysfunction (viability
>
10%). The decision to use 10% as a
cut-off point was informed by findings by Ling
et al
., who found
that revascularisation of patients with hibernating myocardium
that exceeded 10% of the total myocardium was associated with
increased survival, mainly if revascularisation was performed not
later than 92 days after PET imaging.
12
Different study designs and variable interpretation of
perfusion–metabolism images have resulted in conflicting
study outcomes that have caused controversy surrounding the
clinical utility of myocardial viability imaging. For example,
the sub-study of the Surgical Treatment for Ischemic Heart
Failure (STICH) trial failed to show a survival benefit in patients
referred for viability imaging prior to revascularisation. In this
trial, participants were referred for viability imaging with SPECT
and dobutamine stress echocardiography. These modalities have
been reported to have a lower diagnostic accuracy for detecting
myocardial viability when compared to F18-FDG PET.
13
In our study, there were two clinical variables found in the
multivariable regression analysis to be significantly associated
with myocardial viability. Patients on aspirin therapy were
twice as likely to have viable segments. In a meta-analysis
evaluating the benefit and risk of low-dose aspirin in patients
with stable cardiovascular diseases, aspirin was associated with
a 21% reduction in the risk of non-fatal myocardial infarction,
non-fatal stroke and cardiovascular death.
14
The anti-platelet
effect of aspirin in culprit vessel lesions most likely improves
myocardial perfusion and therefore viability.
Hypertension was another clinical variable significantly
associated with myocardial viability. In a recent prospective
study evaluating the role of F18-FDG PET in the assessment
of myocardial viability involving 120 patients with myocardial
contractile dysfunction, Srivatsava
et al
. reported a higher
number of infarcted segments in hypertensive patients (
p
=
0.0005).
15
This is in contrast to our study findings, where
hypertensive patients were almost twice as likely to have viable
segments compared to patients without hypertension. We were
unable to find a plausible explanation for this association.
All challenges and limitations associated with retrospective
analysis of data apply in this study. Other relevant clinical
parameters such as atrial fibrillation, high sensitivity C-reactive
protein and a lipid profile were not available. Despite these
limitations, our pilot study demonstrates that in the clinical
management of patients with ischaemic heart disease referred
for PET evaluation, there is a cohort of patients with hibernating
or viable myocardium. Whether the clinical utility of PET has
a significant impact on cardiovascular outcomes remains to be
evaluated.
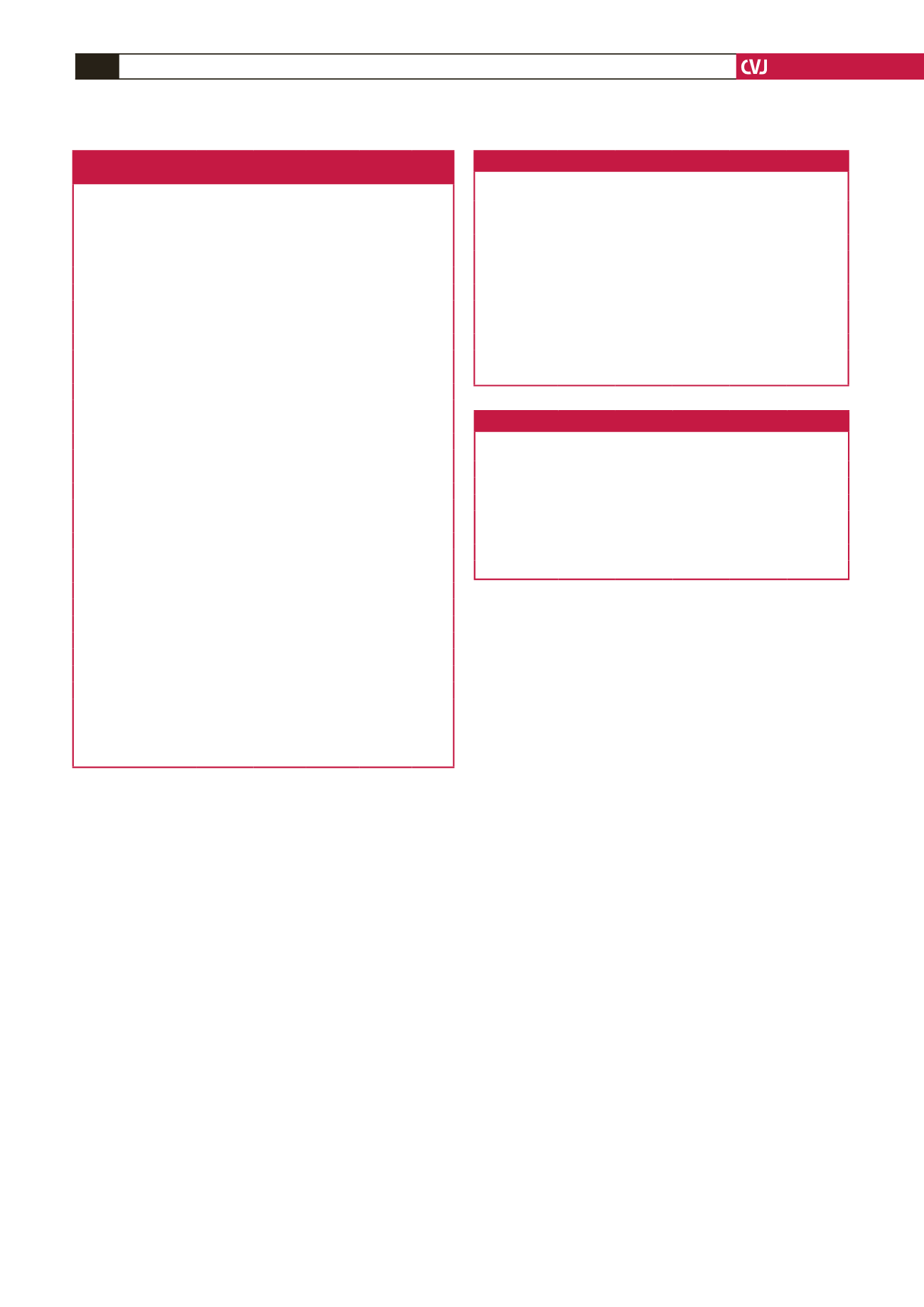
Table 1. Baseline characteristics of patients
according to myocardial viability
Variable
Overall
population
(
n
=
236)
No viabil-
ity, 0%
(
n
=
91)
(38.6%)
Viability,
1
–
10%
(
n
=
14)
(5.9%)
Viability,
>
10%
(
n
=
131)
(55.5%)
p
-value
Male,
n
(%)
196 (83.1) 75 (82.4) 11 (78.6)
107
(81.7)
0.613
Ethnicity,
n
(%)
0.156
Caucasian
125 (53.0) 56 (61.5) 7 (50.0) 62 (47.3)
Indian
71 (30.1) 21 (23.1) 7 (50.0) 43 (32.8)
Black
32 (13.6) 12 (13.2) 0 (0.0)
20 (15.3)
CV risk factors,
n
(%)
Hypertension
115 (48.7) 33 (36.3) 10 (71.4) 72 (55.0) 0.005
Diabetes mellitus
62 (26.3) 17 (18.7) 5 (35.7) 40 (30.5) 0.101
Dyslipidaemia
93 (39.4) 29 (31.9) 11 (78.6) 53 (40.5) 0.004
Smoking
93 (39.4) 35 (38.5) 8 (57.1) 50 (38.2) 0.375
Family history
59 (25.0) 17 (18.7) 6 (42.9) 36 (27.5) 0.093
HIV
4 (1.7)
2 (2.2)
0 (0.0)
2 (1.5)
0.818
Medication,
n
(%)
Beta-blocker
108 (45.8) 31 (34.1) 6 (42.9) 71 (54.2) 0.012
Aspirin
104 (44.1) 29 (31.9) 8 (57.1) 67 (51.2) 0.010
Statin
100 (42.4) 29 (31.9) 8 (57.1) 63 (48.1) 0.028
ACE inhibitor
81 (34.3) 26 (28.6) 5 (35.7) 50 (38.2) 0.332
Ca
2+
antagonists
65 (27.5) 20 (22.0) 1 (7.1)
44 (33.6) 0.035
Nitrates
46 (19.5) 14 (15.4) 4 (28.6) 28 (21.4) 0.366
Wall motion,
n
(%)
Akinesia
65 (27.5) 29 (31.9) 2 (14.3) 34 (26.0) 0.324
Dyskinesia
80 (33.9) 24 (26.4) 5 (35.7) 51 (38.9) 0.149
Global hypokinesia
124 (52.5) 49 (53.9) 9 (64.3) 66 (50.4) 0.582
LVEF (SPECT),
n
(%)
Preserved (≥ 50%)
15 (6.4)
4 (4.4)
3 (21.4)
8 (6.1)
0.027
Mid-range (40–49%)
32 (13.6) 6 (6.6)
2 (14.3) 24 (18.3)
Reduced (
<
40%)
183 (77.5) 77 (84.6) 9 (64.3) 97 (74.1)
Data are shown as absolute numbers and (percentage) for categorical variables.
CV: cardiovascular; CAD: coronary artery disease; HIV: human immunodefi-
ciency virus; Ca
2+
: calcium; ACE: angiotensin converting enzyme; SPECT: single-
photon emission computed tomography; LVEF: left ventricular ejection fraction.
Family history refers to history of any cardiovascular disease.
Table 2. Univariable logistic regression
Odds ratio Std error
z
p
-value
Confidence
interval
LVEF ≤ 39% 2.25
1.98
0.93
0.354 0.40–12.6
LVEF 40–49% 6.00
5.74
1.87
0.061 0.92–39.2
LVEF ≥ 50% 2.29
2.30
0.82
0.413 0.32–16.5
Dyskinesia
1.67
0.47
1.82
0.069 0.96–2.91
Hypertension
1.76
0.47
2.13
0.033 1.04–2.96
Aspirin
1.92
0.52
2.43
0.015 1.13–3.26
Male
0.98
0.33
–0.04
0.964 0.51–1.92
Diabetes
1.68
0.51
1.65
0.098
0.91–3.02
Dyslipidaemia
1.10
0.30
0.37
0.712 0.65–1.87
Smoking
0.89
0.24
–0.43
0.664 0.52–1.50
LVEF: left ventricular ejection fraction; std error: standard error.
Table 3. Multivariable logistic regression
Odds ratio Std error
z
p
-value
Confidence
interval
LVEF ≤ 39% 1.90
1.70
0.71
0.478 0.33–11.0
LVEF 40–49% 4.90
4.91
1.58
0.113 0.68–34.9
LVEF ≥ 50% 3.87
4.13
1.27
0.205 0.48–31.3
Dyskinesia
1.66
0.51
1.64
0.102 0.90–3.04
Hypertension
1.89
0.55
2.19
0.029 1.07–3.33
Aspirin
1.92
0.56
2.23
0.026 1.08–3.41
LVEF: left ventricular ejection fraction; Std error: standard error.



















