
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 6, November/December 2019
344
AFRICA
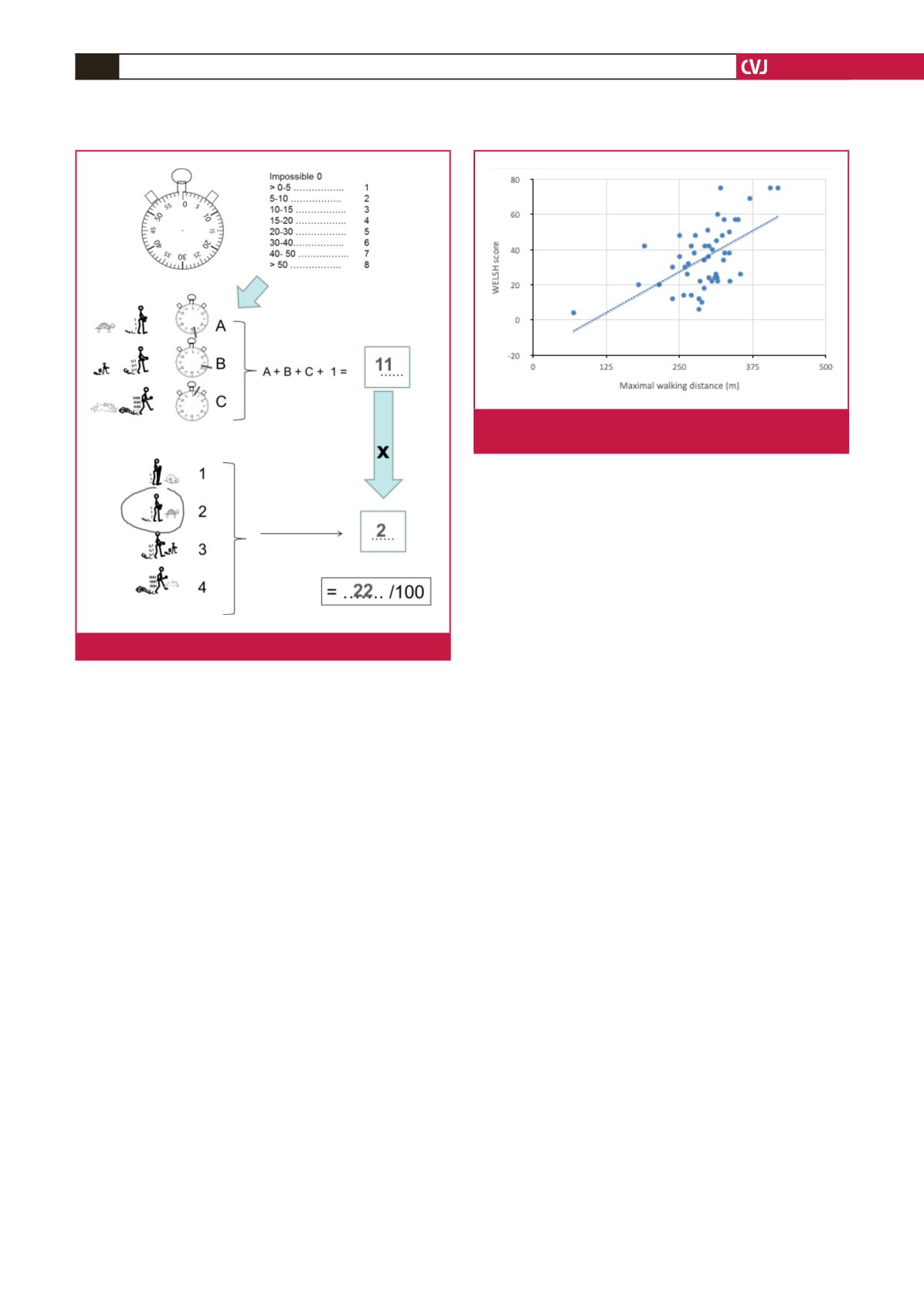
the WELSH tool without errors and the other 16 patients
(32.6%) made errors on one or more of the four items, with a
median number of errors of two items, mainly in the first three
items dealing with the duration of each task. Most of these
errors related to a paradoxical increase in the duration that
could be sustained for a walking speed with an increase in task
difficulty, and were corrected after discussion with the patients.
The WELSH scores were calculated for all patients and the
mean was 35
±
17. An example of scoring is presented in Fig.
2. In this example, the subject reported he/she was able to walk
for a maximum of approximately 23 minutes at a ‘slow’ speed
(five points), approximately 17 minutes at a ‘normal’ speed (four
points) and approximately three minutes at a ‘fast’ speed (one
point) and reported he/she walked slower (turtle) than other
people (coefficient = 2). The final score was 22 = [(5
+
4
+
1)
+
1]
×
2 (Fig. 2).
No adverse event occurred during the six-minute walk test.
The mean maximal walking distance was 292
±
57 m.
The step-by-step multilinear regression analysis stopped
at step one with the WELSH score being the sole predictor
of MWD (
r
= 0.68,
p
<
0.001) and the model being MWD =
1.99
×
score
+
224 m. None of the other variables introduced
in the model (gender, age, school level, body mass index, waist
circumference, NYHA class) reached statistical significance for
the association with MWD, as shown in Fig. 3.
Discussion
This is the first ever reported standard tool developed to
facilitate and standardise the estimation of walking disability
in illiterate patients. The feasibility of the WELSH tool is
relatively high, keeping in mind that half of the self-completed
walking impairment questionnaires (the most widely used tool
to estimate walking impairment) need correction.
19
The WELSH
tool is easily scored and its correlation with objectively measured
maximal symptom-limited walking distance and the six-minute
maximal walking distance was good.
Beyond the obvious interest in a tool for non-literate children
or illiterate adults, developing a tool to score walking disability
based on only drawing could also be valuable to eliminate
language differences in questionnaire translations. What is
of particular interest is that the proportion of our patients
attending primary and secondary school was in the range of
literacy estimated for the Burkinabe population.
20
Indeed, using
a questionnaire in a language that is different from the language
in which it was initially developed is a complex process, requiring
cross translation and validation in the new language.
9,10,21-23
Whether or not the WELSH tool can be used in a context other
than the African population remains to be studied.
We underscore here that the drawings were chosen on
purpose with animals that are present worldwide. Specifically,
when developing the WELSH tool, the fast speed was initially
suggested to be an antelope but these animals are not present in
all countries (e.g. America or Australia).
Another issue to be solved was the representation and
estimation of time. With digital watches, classic watch screens
may gradually disappear, and the selection of patients able to
read a classic clock/watch screen may have biased our results.
24
In fact very few patients, except those with cognitive disorders,
were excluded because of their inability to read a watch. This
might partly be due to the use of watches and clocks for
religious purposes because of a high proportion of Islamic
patients in Burkina Faso.
20
A second question was whether or
not numbers should be added on the clock. Adding Western
type (Arabic) numbers may have facilitated the completion of the
questionnaire, and these can easily be converted to other types
(e.g. Roman or Chinese) with no ambiguity.
The WELSH tool can provide additional information to
the six-minute walking test about the self-reported impairment
in the community, keeping in mind that the six-minute test is
performed at a forced pace,
25
and not at the usual pace of the
patient. Furthermore, the WELSH tool should not replace the
Fig. 2.
Example of scoring sheet for the WELSH tool.
Fig. 3.
Scatterplot of WELSH score and maximal walking
distance.



















