
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 4, July/August 2020
202
AFRICA
Statistical analysis
Continuous variables are presented as means ± standard
deviation (± SD) or median (interquartile range). Categorical
data are presented as proportions. For statistical comparisons
between groups, we used the Student’s
t-
test for continuous
variables and Pearson’s chi-squared test or Fisher’s exact test
for categorical variables. We used Epi Info 3.5.8 (CDC, Atlanta,
USA).
Results
Among a total of 780 patients hospitalised for STEMI [median
delay 20 hours (5–72 hours)], 471 were admitted within 48 hours
of the onset of symptoms. Fibrinolysis was performed in 102
patients within 12 hours of the onset of symptoms. One-hundred
and sixty six patients underwent primary PCI, with a ratio of
primary PCI/STEMI of up to 21.3%.
Mean age was 54.5 years and 91.6% were men. Main risk
factors were hypertension (49.4%) and active smoking (34.3%).
One hundred and six patients (63.9%) were admitted within 12
hours of the onset of symptoms and 38 (22.9%) between 12 and
48 hours, 27.1% presented with Killip class II or higher initially
(Table 1).
The location of MI was anterior in 56.6% of STEMI patients.
Left ventricular systolic depression was found in 16.9% of cases
(Table 1).
The femoral approach was the most commonly used (78.3%)
compared to 21.7% for the radial approach. One-vessel coronary
artery disease (CAD) was observed in 56% of cases (Table 2).
All patients received a loading dose of aspirin of 150–300
mg intravenously (iv) or orally. The P2Y12 inhibitor given was
clopidogrel 300–600mgorally in96.4%of cases. Ticagrelor 180mg
was given to six patients (3.6%). A daily dual antiplatelet therapy
regimen (aspirin + P2Y12 inhibitor) was implemented usually
for up to 12 months after the PCI procedure. Anticoagulant
options were iv bolus of unfractionated heparin 70–100 UI/kg
or enoxaparin 0.5 mg/kg.
Primary PCI was performed with stent implantation in
84.3% of patients. Bare-metal stents (BMS) were the most
frequently used stents (57.9%). Drug-eluting stents (DES)
were less frequently used (42.1%) (Table 2). In most cases,
angiographic success was observed (157/166, 94.6%). Non-fatal
complications were mainly haematomas (6/166, 3.6%). Peri-
procedural mortality rate was 1.2% (2/166).
According to the time of admission, our population study
was divided into two groups: group 1 (≤ 12 hours) and group
2 (13–48 hours). PCI failure significantly occurred in group 2
(13.3 vs 0.9%,
p
< 0.001). Table 3 summarises the key in-hospital
outcomes between groups. Congestive heart failure was mostly
reported in patients admitted over 12 hours (38.3 vs 20.8%,
p
= 0.01). Although there was no statistical difference, a trend
was observed concerning left ventricular systolic depression
occurrence in patients admitted over 12 hours (23.3 vs 13.2%,
p
= 0.09).
Discussion
As the incidence of ACS increases in sub-Saharan Africa,
implementationof primaryPCI remains a challenge. Sub-Saharan
African countries have limited access to heart centres where PCI
can be performed. Few catheterisation laboratories with routine
procedures and trained interventional cardiologists are available
across sub-Saharan Africa.
6-11
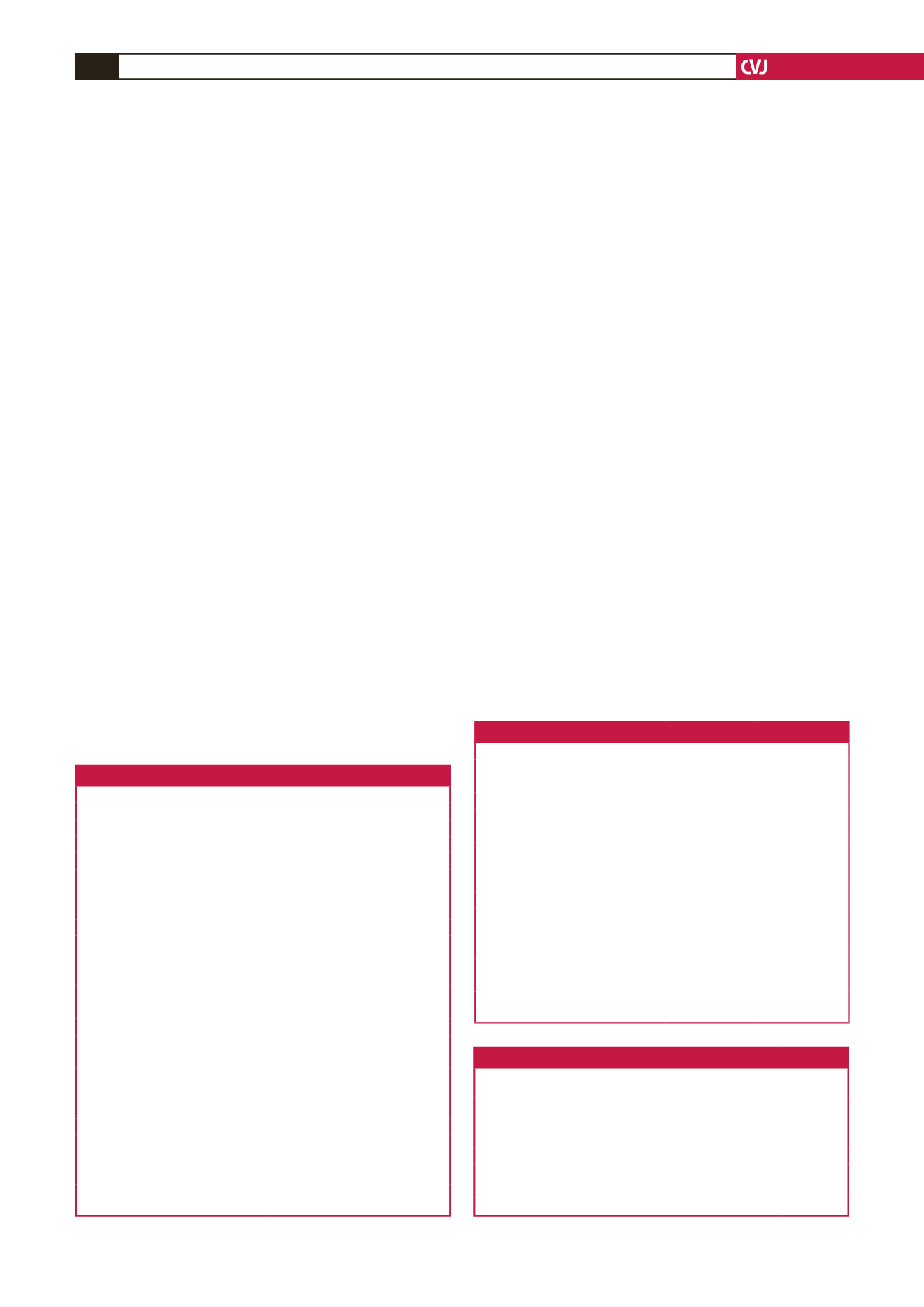
Table 1. Baseline characteristics of the study population
Number (166)
Percentage
Risk factors and history
Age (years), mean ± SD
54.5 ± 10.5
Male gender
152
91.6
Hypertension
82
49.4
Diabetes
41
24.7
Active smoking
57
34.3
Dyslipidaemia
51
30.7
Familial history of CAD
17
10.2
Previous PCI
20
12.0
Delay from onset to admission (hours)
≤ 12
106
63.9
13–24
38
22.9
24–48
22
13.2
Killip class
I
121
72.9
II
26
15.7
III
11
6.6
IV
8
4.8
Location of STEMI
Anterior
94
56.6
Inferior
61
36.8
Lateral
11
6.6
LVEF < 40%
28
16.9
CAD: coronary artery disease, PCI: percutaneous coronary intervention, STEMI:
ST-elevation myocardial infarction, LVEF: left ventricular ejection fraction.
Table 2. Procedures and management
Number (166)
Percentage
Vascular access
Femoral
130
78.3
Radial
36
21.7
Severity of CAD
1-vessel disease
93
56.0
2-vessel disease
46
27.7
3-vessel disease
27
16.3
Left main
4
2.4
PCI procedure
Stenting
140
84.3
Ballon angioplasty
26
15.7
Type of stent (
n =
140)
BMS
81
57.9
DES
59
42.1
CAD: coronary artery disease, PCI: percutaneous coronary intervention, BMS:
bare-metal stent, DES: drug-eluting stent.
Table 3. In-hospital outcomes according to time of admission
Outcome
≤ 12 hours
(
n
= 106)
13–48 hours
(
n
= 60)
p
-value
Congestive heart failure,
n
(%)
22 (20.8)
23 (38.3)
0.01
Ventricular tachycardia,
n
(%)
3 (2.8)
1 (1.7)
1.00
Atrial fibrillation,
n
(%)
1 (0.9)
1 (1.7)
1.00
High-degree AV block,
n
(%)
2 (1.9)
1 (1.7)
1.00
LVEF < 40%,
n
(%)
14 (13.2)
14 (23.3)
0.09
Death,
n
(%)
1 (0.9)
1 (1.7)
1.00
AV: atrio-ventricular, LVEF: left ventricular ejection fraction.



















