
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 4, July/August 2020
208
AFRICA
commonly in the medical field as a surrogate measurement of
global kidney functioning.
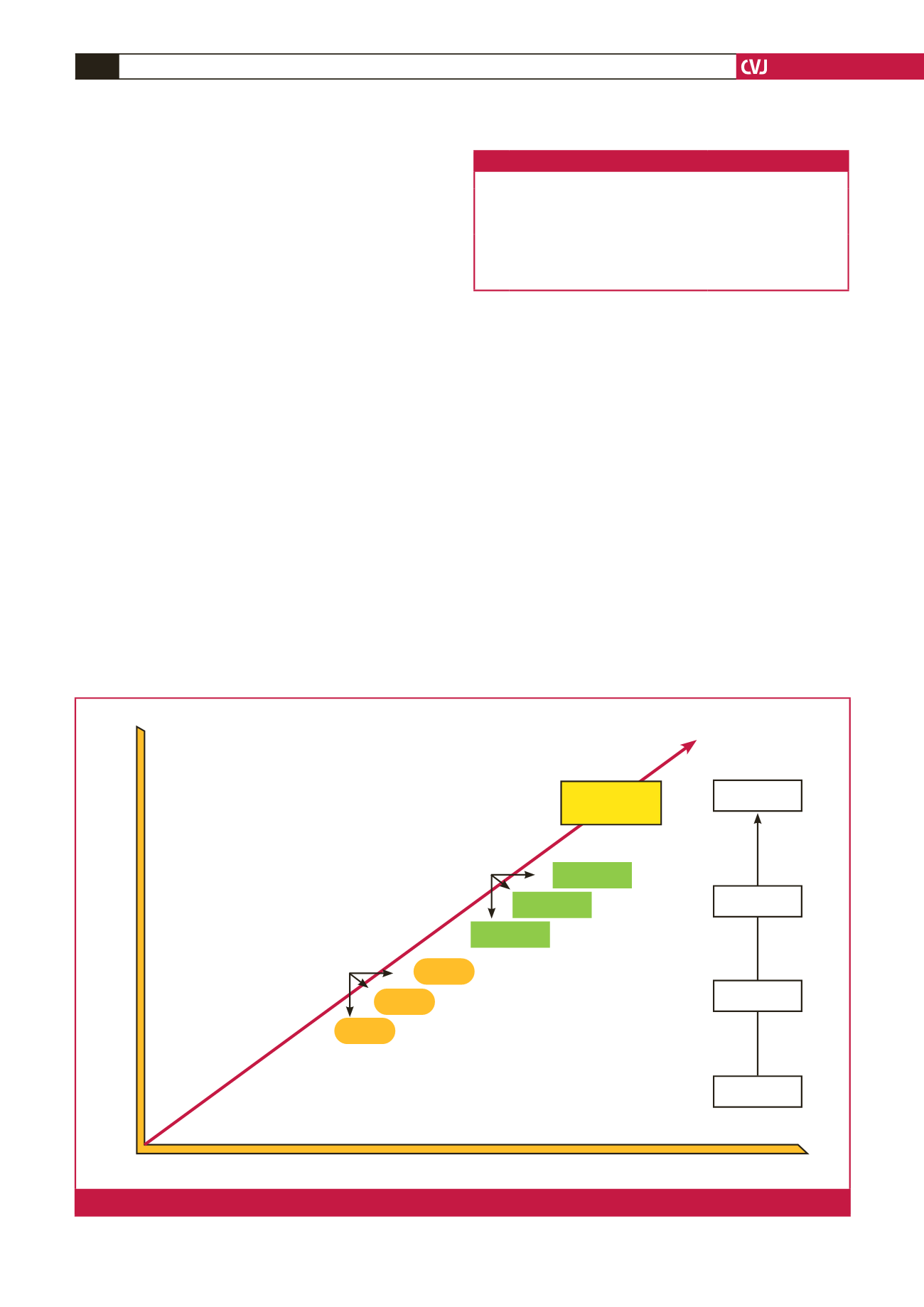
The diagnosis of CSA-AKI has evolved with time. Ronco
44
described what she calls the ‘evolution of AKI diagnostic
syntax’, as shown in Fig. 1. She illustrated how between the years
1950 and 2016, the diagnosis of AKI had evolved from being
a clinical finding to the development of molecular biomarker
tests.
44
Studies have been performed that compare the differences
in the diagnosis of AKI using serum creatinine levels to urine
output volumes.
Criteria for diagnosis of AKI
In 2004, the Acute Dialysis Quality Initiative (ADQI) group
described the RIFLE kidney disease criteria to classify the
diagnosis of AKI.
45
An increase in a RIFLE score stage was
shown to lead to an increase in the risk of death.
5
The RIFLE
criteria utilised serum creatinine levels or GFR, and the patient’s
urine output to stratify them into risk, injury, failure and loss, or
end-stage kidney disease grades according to the duration and
loss of their renal function.
14
The RIFLE criteria are known to
follow up the changes in renal function as observed over a period
of seven days.
45
The AKIN was subsequently developed as a modification
of the RIFLE criteria by decreasing the threshold of serum
creatinine levels in the first 48 hours of the diagnosis of AKI.
9
The AKIN further classified patients that require RRT into
AKIN stage 3 and removed eGFR criteria as part of their
work-up. Regardless of their differences, the RIFLE and AKIN
classification criteria have proven to be useful in identifying
patients with AKI.
9
In 2013, the international AKI guideline work group brought
together international experts from several medical specialities
to produce a uniform definition and classification of AKI, as
well as prevention strategies, pharmacological treatment and
RRT guidelines.
5,46
This programme standardised the definition
of AKI by bringing together the RIFLE and AKIN criteria and
producing the KDIGO criteria for AKI.
46
AKI by KDIGO is defined as an increase in serum creatinine
of ≥ 0.3 mg/dl (or 26.5 µmol/l) for a period of ≤ 48 hours, or a
rise in serum creatinine of ≥ 1.5-fold from the baseline, which
is presumed to have occurred in the preceding seven days.
9
The
diagnosis, evaluation and management of AKI, a KDIGO
summary, divides AKI into three stages as illustrated in Table 1.
5
Table 2 demonstrates the differences in AKI diagnosis between
the RIFLE score, and AKIN and KDIGO criteria.
7
In the KDIGO criteria, patients with AKI can be diagnosed
by solely using serum creatinine levels. This criterion has been
shown to be a good predictor of 30-day mortality rate in patients
1950
2000
1980
2013
2016
(Years)
2010
Quality of AKI diagnosis
Definition &
Classification
Diagnosis
Oliguria
Uraemia
35 ARF
definitions
RIFLE
AKIN
KDIGO
Pathophysiological understanding of AKI
Clinical
Severity
Mechanisms
Conceptual model
ARF
≠
ATN
ARF
Stage 1
Stage 2
Stage 3
Failure
Injury
Risk
AKI risk
Kidney stress
Subclinical AKI
Molecular
Cellular
Biochemical
Clinical
Fig. 1.
The evolution syntax of AKI diagnosis by Ronco.
44
Table 1.The staging of AKI according to Kellum
et al.
5
Stage Serum creatinine
Urine output
1
1.5–1.9 times baseline within 1 week or
≥ 0.3 mg/dl increase within 48 hours
<
0.5 ml/kg/h for 6–12 hours
2
2.0–2.9 times baseline
<
0.5 ml/kg/h for ≥ 12 hours
3
3.0 times baseline or increase in serum
creatinine to ≥ 4.0 mg/dl or the initia-
tion of RRT or in patients
<
18 years, a
decrease in eGFR to
<
35 ml/min/1.73 m
2
<
0.3 ml/kg/h for ≥ 24 hours
or anuria for ≥ 12 hours



















