CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 1, January/February 2010
10
AFRICA
than creatinine clearance rate.
4
The simplified MDRD (sMDRD)
equation uses only age, gender, race and s-creatinine value.
The accuracy compares favourably with the standard MDRD.
5
Estimated GFR from the sMDRD can easily be given with an
s-creatinine request from the laboratory.
The application of calculated GFR has been noted in the
cardiac surgical literature.
6
A strong correlation was found
between the varying degrees of renal dysfunction pre-operatively
and adverse events after cardiac surgery. The purpose of our
study was to investigate the association between calculated GFR
pre-operatively and renal impairment postoperatively in a local
setting. In the literature, the Cockcroft and Gault formula has
been used more widely, but for this study, the sMDRD method
was applied. This gave us an opportunity to simultaneously estab-
lish the prevalence of renal impairment in a local population with
so-called normal kidney function according to s-creatinine levels.
Methods
The target population included all patients who had a coronary
artery bypass graft operation done by one surgeon in one hospi-
tal between January 2005 and October 2007. All patients had
their operations performed on cardiopulmonary bypass with
non-pulsatile flow at moderate systemic temperature and with
cardioplegic cardiac arrest. Patients who were on renal dialysis
beforehand, off-pump bypass surgery (OPCAB) cases, CABG
cases with an additional cardiac procedure, and those who died
intra-operatively were excluded.
S-creatinine levels were determined automatically with the
Jaffe method in a Synchron LX
®
system with the normal range
between 80 and 130
μ
mol/l. The patient’s age, gender and
s-creatinine value were used with a computer desktop calculator
to determine the GFR according to the formula for sMDRD:
7
GFR (ml/min/1.73m
2
) = 186
×
(S-Cr)
1.154
×
age
0.203
×
0.742 (if
female)
×
1.21 (for black race group)
Pre-operative patients were grouped into the five stages of
chronic kidney disease (CKD) as defined by the National Kidney
Foundation (NKF)
8
(Table 1). For purposes of this study, postop-
erative renal impairment was defined as a 50% rise in the pre-
operative s-creatinine level, with or without renal dialysis.
9
Other information obtained from patient records included the
EuroSCORE, presence of diabetes mellitus, left ventricular ejec-
tion fraction (LVEF) less than 40%, mediastinal drainage, usage
of homologous blood, length of hospital stay (LOS) and mortal-
ity. The data were analysed by the Department of Biostatics at
the University of the Free State. Numerical data are expressed as
means. Categorical variables are indicated in percentages. Possible
differences in percentages were calculated. The association
between stage of renal impairment before and after the operation
was calculated as a relative risk with 95% confidence interval.
This study was approved by the Ethics Committee of the
Faculty of Health Sciences at the University of the Free State,
Bloemfontein, and the Board of the Bloemfontein Medi-Clinic
Hospital.
Results
After the exclusion criteria were applied, 451 patients were
available for the study. The mean age was 60.5 years with a
male:female gender distribution of 339:112 (75.2:24.8%). Of
these patients, 98 (21.7%) had diabetes mellitus. Twenty-one
patients (4.7%) had a left ventricular function of less than 40%
ejection fraction. As a group, the additive EuroSCORE for
operative risk for mortality was 3.26%. The mean estimated GFR
using the sMDRD was 74.7 ml/min/1.73m
2
. The patients were
categorised into the five stages of chronic kidney disease (CKD).
None fell into stage 5; the majority of patients (283 or 62.7%)
had stage 2 kidney disease (Table 2).
Table 3 shows the outcome of patients based on their pre-
operative renal function. Acceptable kidney function was found
in 365 patients (80.9%), but 86 (19.1%) had, per definition,
chronic kidney disease (stages 3 and 4) prior to CABG. These
patients with chronic kidney disease were older and had a higher
operative risk with a mean EuroSCORE of 4.7 vs 2.9% for those
with reasonable kidney function. The mediastinal blood losses
measured over 48 hours were almost the same (mean 691 ml
for those with CKD vs 700 ml in those with reasonable kidney
function), but the necessity for homologous blood was higher
in the impaired group (mean 1.1 vs 0.5 units per patient). The
healthier patients stayed in hospital on average one day less than
those with kidney failure. The mortality for the two groups was
five patients (1.4%) with normal kidneys before the operation
and two (2.3%) for those with prior CKD. This difference did not
reach statistical significance.
After the operation the patients were again classed in two
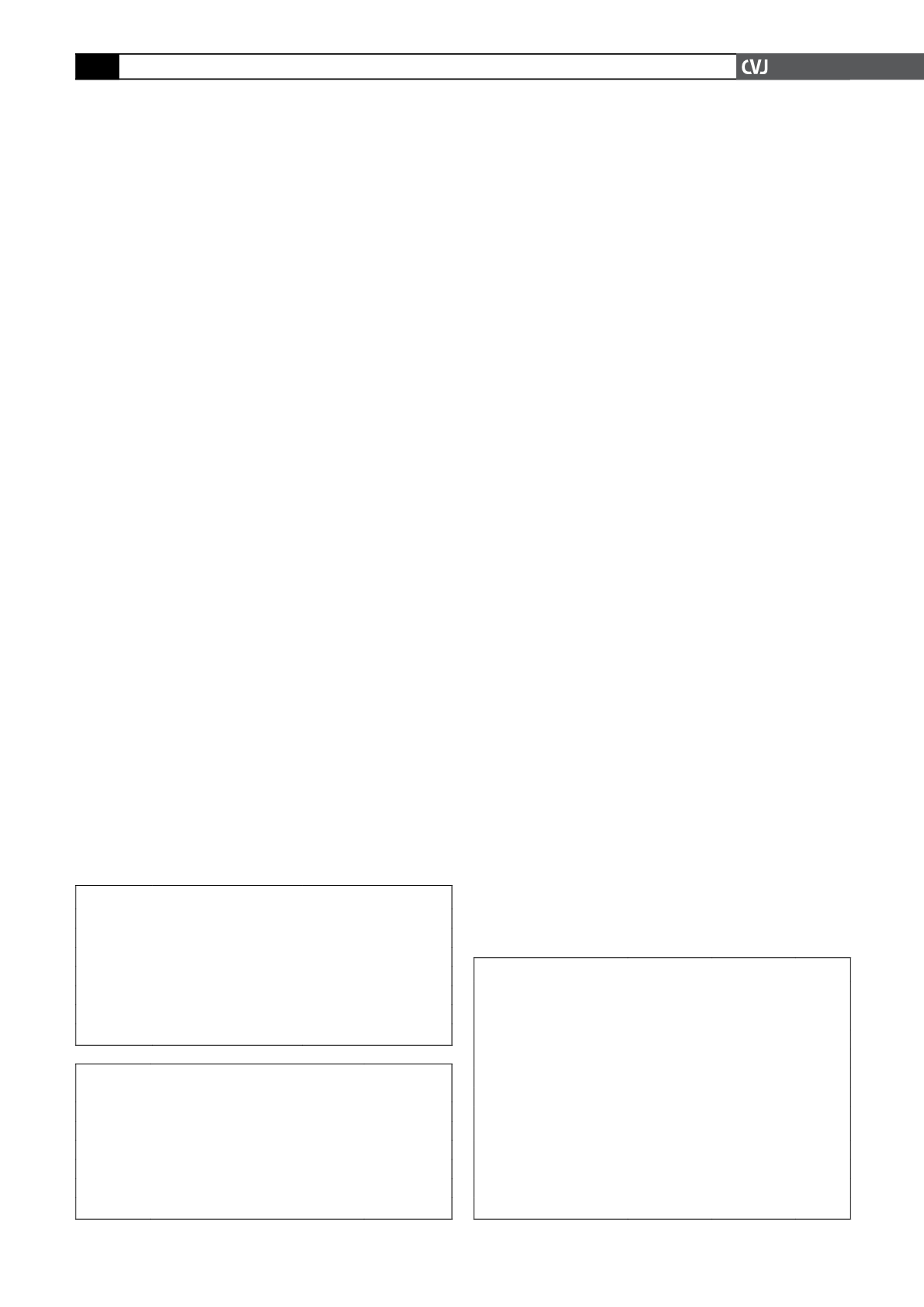
TABLE 1. STAGES OF CHRONIC KIDNEY DISEASE
CKD stage
Description
GFR (ml/min/1.73 m
2
)
1
Normal
≥
90
2
Mild
↓
in GFR
60–89
3
Moderate
↓
in GFR
30–59
4
Severe
↓
in GFR
15–29
5
Kidney failure
<
15
GFR
=
glomerular filtration rate.
TABLE 2. CHRONIC KIDNEY DISEASEACCORDINGTO
GFR BASED ON sMDRD
CKD stage
GFR (ml/min/1.73 m
2
)
Patients
n
(%)
1
>
90
82 (18.2)
2
60–89
283 (62.7)
3
30–59
83 (18.4)
4
15–29
3 (0.7)
5
<
15
0 (0.0)
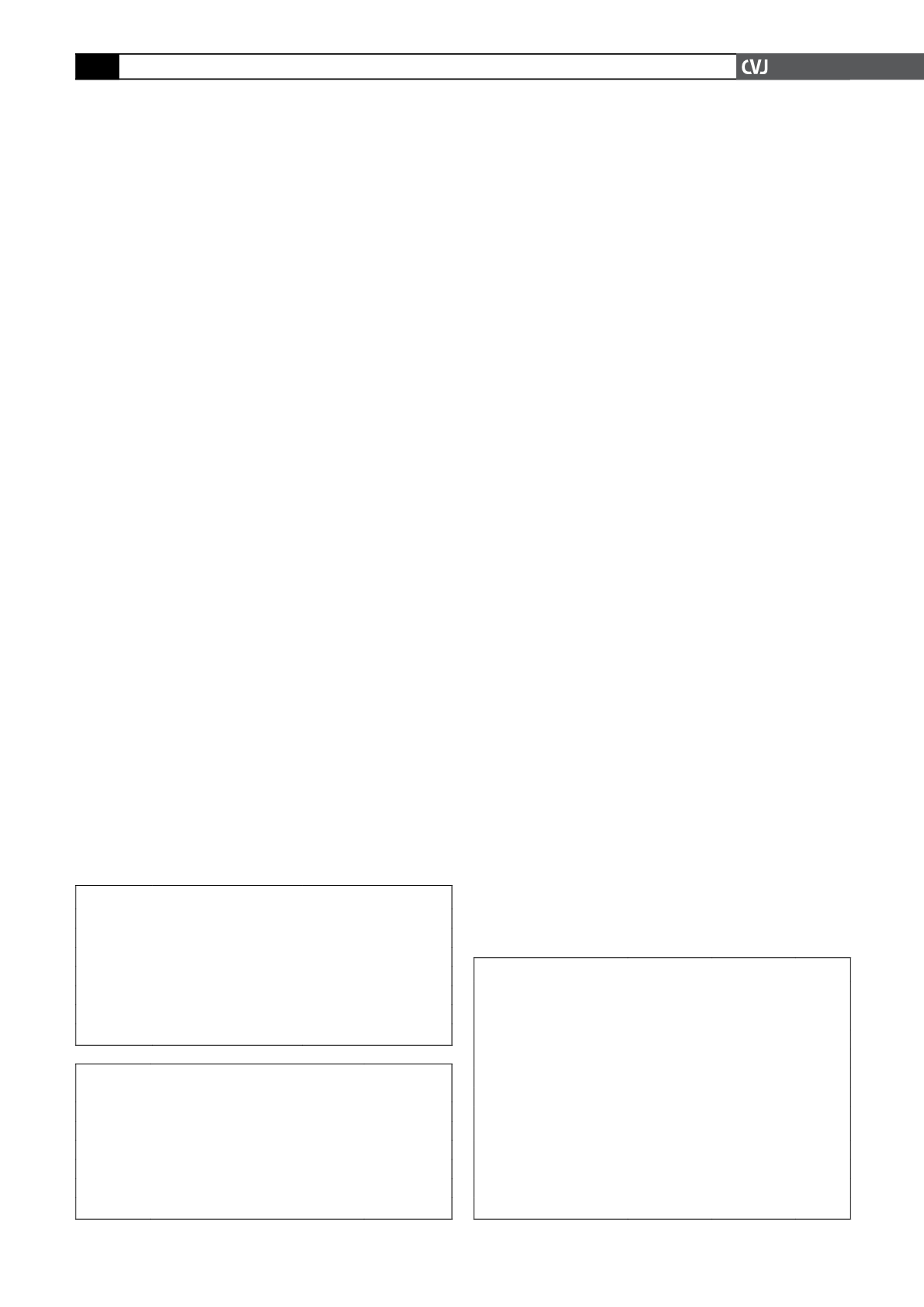
TABLE 3. KIDNEY FUNCTION PRE-OPERATIVELY
GFR
>
60 ml/
min/1.73 m
2
(%)
GFR
<
60 ml/
min/1.73 m
2
(%)
p
Patients
365 (80.9)
86 (19.1)
Mean age (years)
59.3
65.6
<
0.0001
Mean EuroSCORE
2.9
4.7
<
0.0001
Mean mediastinal loss (ml)
700
691
0.9117
Mean homologous blood
(units/patient)
0.5
1.1
<
0.0001
Post-op
↓
kidney function
14 (3.8)
20 (23.3)
<
0.0001
Mean LOS days (days)
5.6
6.8
<
0.0001
Mortality
5 (1.4)
2 (2.3)
0.6229
GFR
=
glomerular filtration rate; LOS
=
length of hospital stay.