CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 1, January/February 2010
AFRICA
11
groups; 417 patients (92.5%) did not have a 50% or more increase
in their baseline s-creatinine levels, whereas 34 patients (7.5%)
had more than a 50% increase in baseline s-creatinine (Table
4). The two groups differed in terms of age and EuroSCORE
risk. Those who had renal impairment postoperatively had a
lower pre-operative GFR (mean 55.8 ml/min/1.73 m
2
) compared
to those without any further renal impairment (mean 76.1 ml/
min/1.73m
2
). Eleven (11.2%) patients with diabetes mellitus had
a deterioration of kidney function postoperatively, and 23 (6.5%)
without diabetes had significantly increased s-creatinine levels.
However, this difference did not reach statistical significance.
Left ventricular function did make a difference. Five patients
(23.8%) with a left ventricular function of less than 40% had
renal impairment after the operation, compared to only 29
patients (6.5%) with normal left ventricular function. The length
of hospital stay was longer in those patients with significantly
increased baseline s-creatinine levels (mean 8.1 vs 5.7 days).
The mortality was five (1.2%) patients among those who main-
tained their pre-operative renal function and two (5.9%) who
had further deterioration. This difference was not statistically
significant.
Table 5 summarises the renal outcome of patients as per
stage of CKD. Of the 86 patients who were in stages 3 and 4,
20 (23.2%) had at least a 50% increase in s-creatinine levels
postoperatively, compared to only 14 (3.8%) of the 365 patients
who were in stages 1 and 2 (relative risk 6.1; 95% CI: 3.2–11.5.
One patient with stage 1 renal function had deterioration of his
kidney function. This individual had a serious surgical bleed with
hypotension and a serum haemoglobin of 2 g% soon after arrival
in the intensive care unit, but fortunately he recovered.
Of the 34 patients with renal impairment postoperatively,
three required renal dialysis to correct fluid and electrolyte
imbalances. All three of these patients had s-creatinine values
within the laboratory’s normal range, but with GFR of 43, 46 and
79 ml/min/1.73m
2
, respectively. This last patient who required
dialysis in spite of near-normal pre-operative renal function had
a failed percutanous intervention procedure and was taken to
theatre as an emergency case on an intra-aortic balloon pump. He
was HIV positive due to blood transfusions in the past and also
had raised liver enzymes pre-operatively.
Discussion
Not only is postoperative renal impairment considered a seri-
ous risk factor for adverse effects after CABG, but kidney
disease in itself is a risk factor for coronary artery disease. In
a 10-year study conducted among a group of healthy people
from the general Belgian population, even mild reduction in
GFR was associated with death from coronary artery disease.
10
These patients were exposed to other cardiovascular risk factors
typically associated with coronary artery disease.
11
It is now
advisable that s-creatinine determination as a means of assess-
ing renal function is no longer acceptable and in fact measure-
ment of creatinine clearance using 24-hour urine samples does
not provide a more accurate GFR than do prediction equations.
These two facts are considered level A recommendations.
12
In the present study, renal function was determined with an
estimated GFR based on the sMDRD equation. The Cockcroft
and Gault equation has been used more commonly to address the
association between pre-operative renal function and post CABG
outcome.
13,14
The sMDRD uses only age, gender and s-creatinine
level to calculate an estimated GFR.
All the patients were grouped according to the NKF stages for
kidney function. Only 18.2% had normal kidney function (stage
1). A GFR of 60 ml/min/1.73m
2
was used as cut-off point and
19.1% of patients had chronic renal impairment pre-operatively.
This was surprisingly high as only 11 patients had s-creatinine
values higher than 141
µ
mol/l. The patients with impaired renal
function were older, however the sMDRD takes age into account.
The EuroSCORE uses s-creatinine levels above 200
µ
mol/l as
a mortality risk factor and in this series only two patients fell
into this category, yet the impaired group had a higher risk for
mortality. The higher age would probably explain this; they were
on average six years older, with every five years over 60 years
contributing 1% to the risk score.
Interestingly, the postoperative mediastinal drainage did not
differ much, but the impaired group required more homologous
blood. One would like to believe that kidney dysfunction contrib-
uted to that, but pre-operative haematocrit values were not part of
the study. We could not demonstrate a difference in mortality rate
although this was clear from a large database of patients where
it was demonstrated that operative mortality rate rose inversely
with declining renal function.
15
The two patients who died among
those with pre-operative stages 3 and 4 CKD were the same two
who had postoperative deterioration of baseline s-creatinine
levels. Impaired renal function with further deterioration could
therefore be a risk for mortality. However this hypothesis was not
tested, as the number of patients was too small.
After the operation, the patients’ renal function were
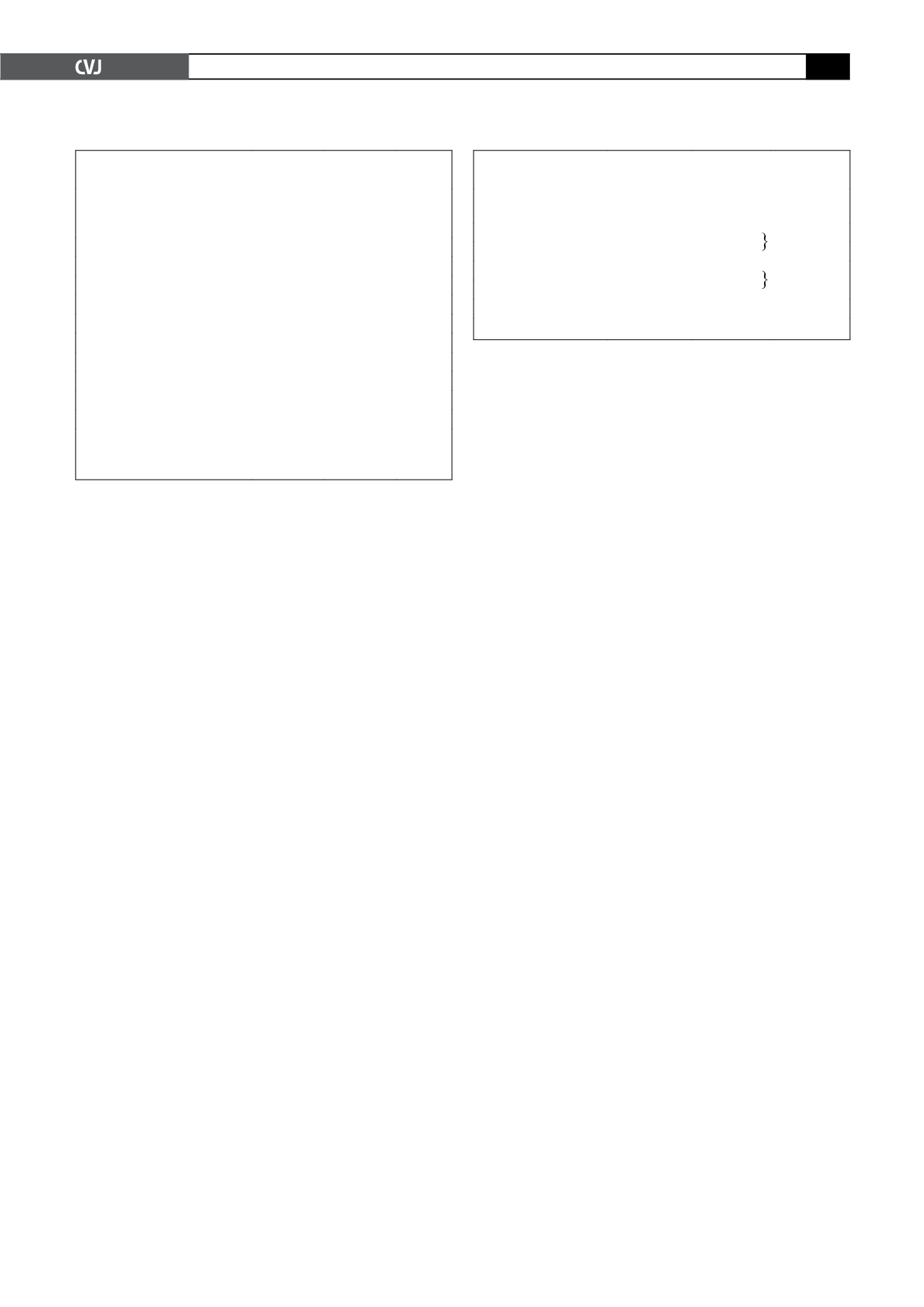
TABLE 4. KIDNEY FUNCTION POSTOPERATIVELY BASED
ON S-CREATININE CHANGE FROM BASELINE
<
50% rise
in Cr
n
(%)
>
50% rise
in Cr
n
(%)
p
Patients
417 (92.5)
34 (7.5)
Mean age (years)
59.8
68.8
<
0.0001
Mean EuroSCORE
3.1
5.1
0.0002
Mean sMDRD (ml/min/1.73m
2
)
76.1
55.8
<
0.0001
DM (
n
=
98)
87 (88.8)
11 (11.2)
0.1183
Non-DM (
n
=
353)
330 (93.5)
23 (6.5)
LVEF
<
40% (
n
=
21)
16 (76.2)
5 (23.8)
0.0153
LVEF
>
40% (
n
=
430)
401 (93.3)
29 (6.7)
Mean LOS (days)
5.7
8.1
<
0.0001
Mortality
5 (1.2)
2 (5.9)
0.0912
Cr
=
creatinine; sMDRD
=
simplified modification of diet in renal
disease; DM
=
diabetes mellitus; LVEF
=
left ventricular ejection
fraction, LOS
=
length of hospital stay.
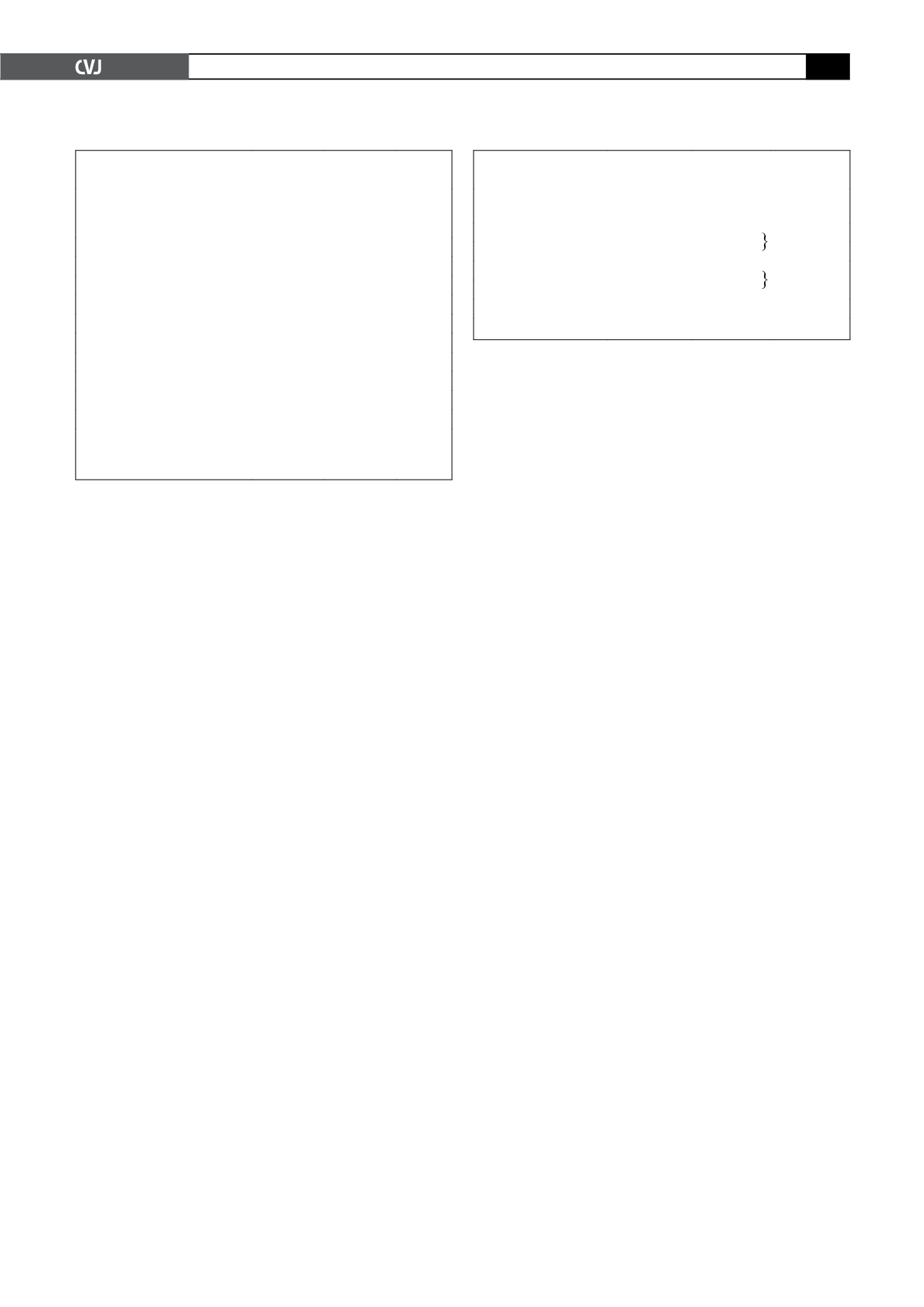
TABLE 5. RENAL IMPAIRMENTACCORDING
TO PRE-OPERATIVE GFR
CKD stage pre-op
Patients
Post-op impairment,
n
(%)
1
82
1 (1.2)
13 (4.6)
14 (3.8)
2
283
3
83
18 (21.7)
2 (66.7)
20 (23.2)
4
3
5
0
CKD
=
chronic kidney disease.