CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 4, May 2013
AFRICA
125
Other factors which have been identified include: the level
of education and training of health workers and/or people with
ARF/RHD who may not fully understand the role of secondary
prophylaxis in preventing ARF and subsequent heart damage;
refusal by some people who do not want to receive treatment
despite their level of understanding; difficulties accessing
healthcare, that is, travelling to the health facility to receive
treatment may be difficult and/or costly, especially for people
living in rural and remote areas; forgetting to attend the health
centre on the date when secondary prophylaxis is due; staff
workloads and priorities. Healthcare staff may be unable to
identify and encourage people who do not receive regular
secondary prophylaxis.
11,12
In Uganda, RHD is the second leading cause of acquired heart
disease after hypertensive heart disease.
13
Current data regarding
adherence rates to secondary benzathine penicillin prophylaxis
among these patients are unknown despite our knowledge
that good adherence is protective for severe forms of RHD.
Therefore, the study aims were (1) to determine the level of
adherence to benzathine penicillin prophylaxis among rheumatic
heart disease patients attending Mulago Hospital, (2) establish
the patient factors associated with adherence and, (3) establish
the reasons for missing monthly benzathine penicillin injections.
Methods
Institutional ethics approval was obtained from the School of
Medicine Research and the Ethics Committee of the College of
Health Sciences, Makerere University. We obtained informed
consent for all the patients and informed assent for those unable
to give consent. Patients’ initials and study numbers were put on
the questionnaires instead of full names to ensure confidentiality.
This was a longitudinal observational study carried out in
Mulago Hospital, the national referral hospital, and Makerere
University teaching hospital located in Kampala, Uganda,
which receives more than 250 patients with RHD annually. The
target population included all patients clinically diagnosed with
rheumatic heart disease and confirmed by echocardiography, as
previously described.
5
New and old RHD patients aged five to 55 years who were
eligible to continue prophylaxis for a period not less than one
year from the time of recruitment and consented to the study
were recruited. Each patient was then given a benzathine
penicillin prophylaxis card recommending the appropriate
monthly (four-weekly) dose of benzathine penicillin according
to the Uganda clinical guidelines, which recommends 2.4 MU
for adults, 0.6 MU for children
≤
30 kg and 1.2 MU for those
>
30 kg.
8
Patients with known allergy to benzathine penicillin were
excluded from the study.
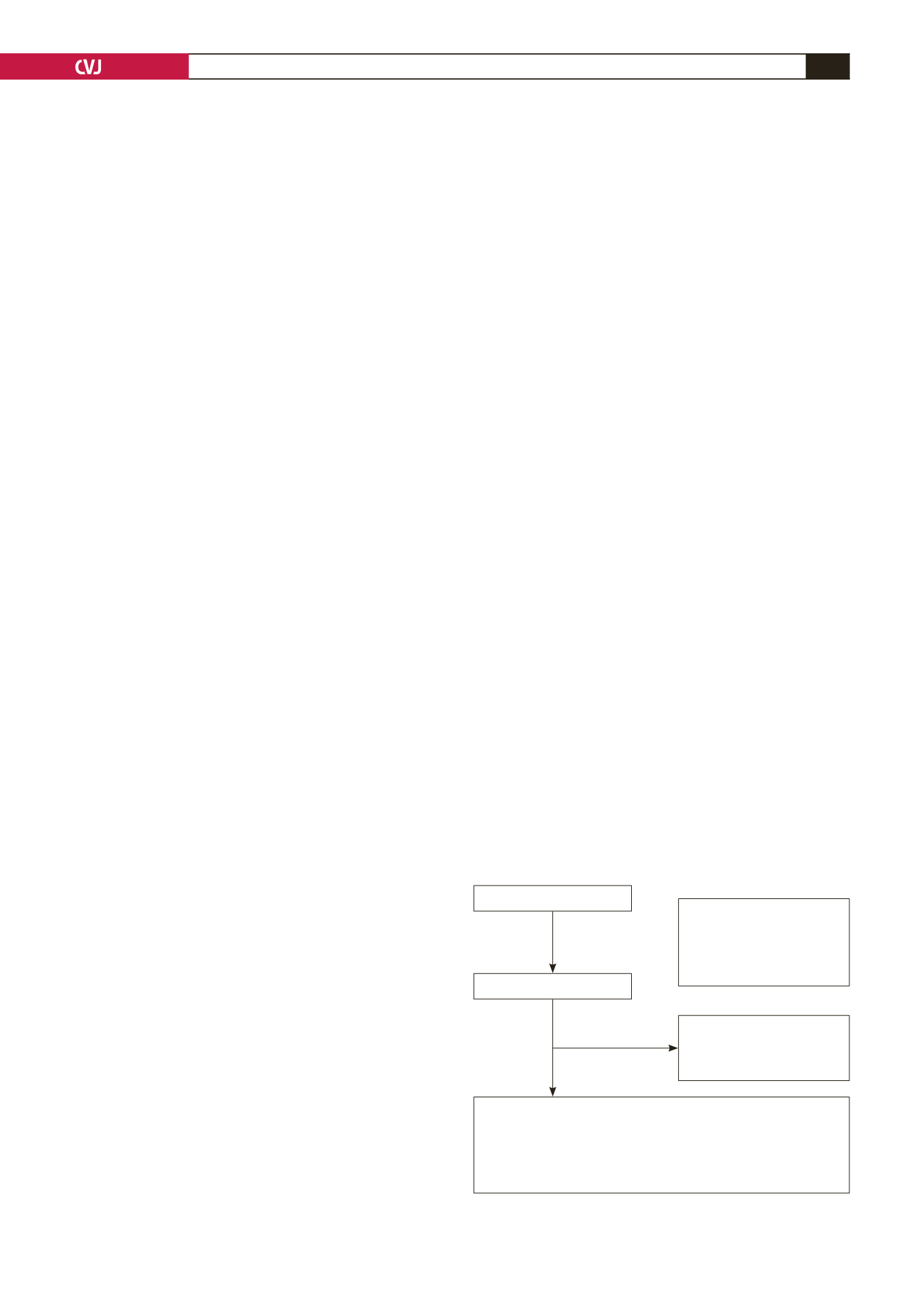
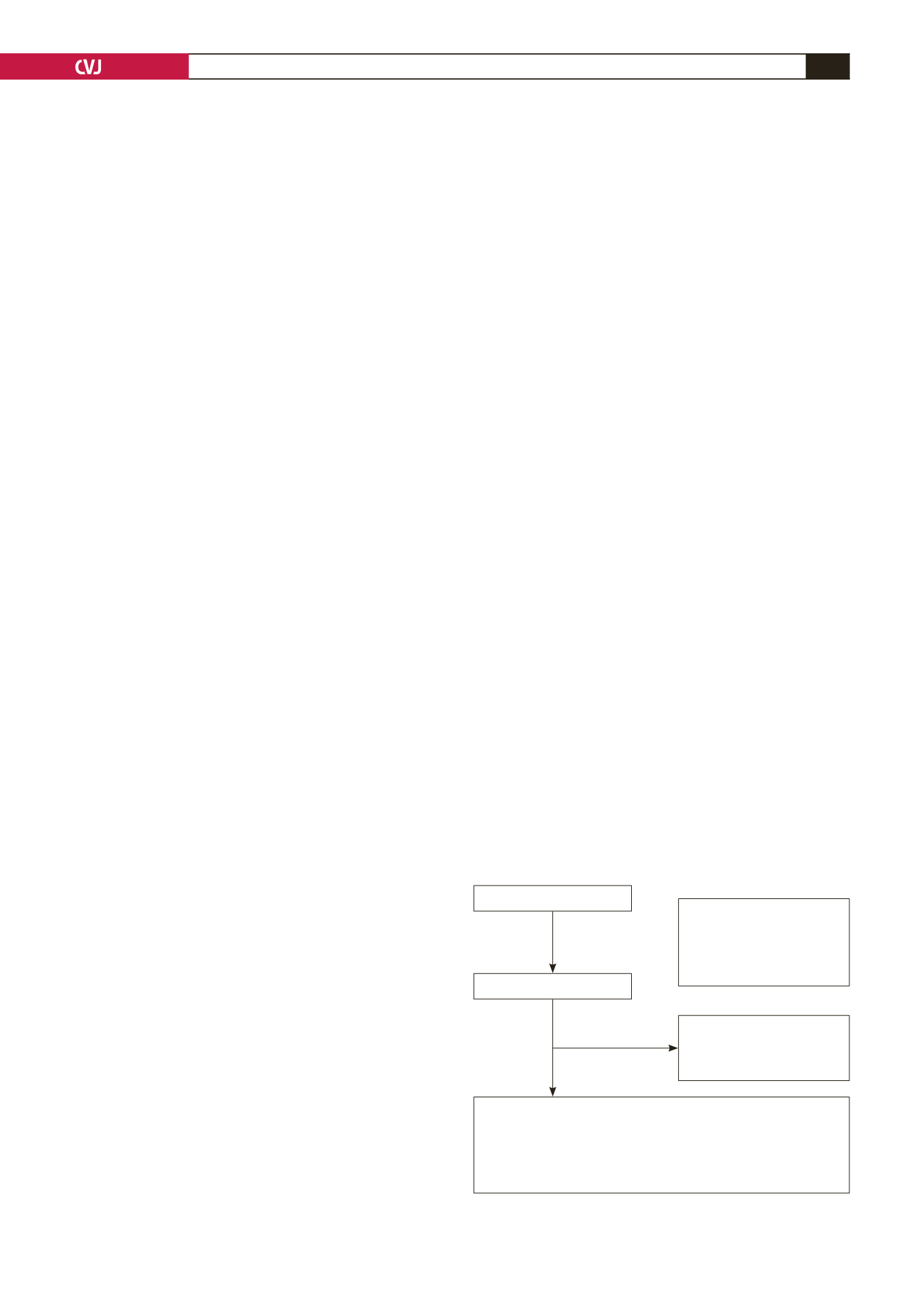
Patients who met the inclusion criteria were consecutively
recruited over a period of four months until a total of 95 patients
was reached (Fig. 1). An identification number or unique
patient number (UPN) was assigned to each consenting patient.
For those who refused to consent, the reason for refusal was
documented in the study book.
A focused clinical assessment was done using a standardised
pre-tested questionnaire in which the socio-demographic data,
details of physical findings, and details of findings on the
electrocardiogram and at echocardiography were recorded. In
addition, data regarding the following were collected: personal
history of hypertension, diabetes, stroke and other heart diseases.
Socio-economic factors recorded were educational level,
occupation, and total income (of parents in the case of children
or students).
For each patient recruited, information regarding the
importance of secondary prophylaxis was provided as part of the
whole information package given to the RHD registry patients,
including all their other treatment modalities. This was done in
liaison with the primary attending clinicians. This was to help
capture the dates and signatures of the health workers where
the patient received the benzathine penicillin injections over
the following six months. The card had the name of the patient,
which would help track the patients’ UPN through the study
book.
For purposes of limiting loss to follow up, data concerning
the following were collected: the patients’ phone numbers if
available/number of the caretaker for children; phone numbers
of at least two close relatives or friends, which would be tested at
the time of recording to ascertain their existence; the number for
the principle investigator was written at the back of each patient’s
benzathine penicillin card, and patients were urged to call and
inform the principle investigator if they were planning to change
their phone numbers.
After recruitment, each patient was told to continue attending
his/her regular clinic, as scheduled by the primary care clinician,
and he/she was to be reviewed in the general RHD registry every
three months by other registry clinicians. For this particular
study, the patients were reviewed again at the end of six months’
follow up.
At the six-month follow-up visit, patients were contacted
by phone and were encouraged to come with their benzathine
penicillin prophylaxis cards so that data regarding their rates of
adherence could be extracted. Those who were unable to travel at
the six-month follow for various reasons were requested to read
off the number of injections received at the time of the call from
the card, and this was recorded in their follow-up questionnaire.
These patients were nevertheless encouraged to take time off and
Fig. 1. Patient flow during the study.
Adherence to benzathine penicillin for secondary
prophylaxis among patients affected with rheumatic
heart disease (RHD) at Mulago Hospital
112 assessed for eligibility
17 ineligible
• 6 probable RHD
• 4 congenital heart disease
• 4 mitral valve prolapse
• 3 refused to consent
95 recruited
13 (13.7%) did not complete
6-month follow up
• 10 died
• 3 lost to follow up
82 (86.3%) completed 6-month follow up
Of these
• 71 (86.6%) had objective assessment of adherence (using the
benzathine card)
• 11 (13.4%) self-reported adherence (6 had lost card upon the
visit and 5 followed up over the phone.)