CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 5, June 2013
186
AFRICA
times, there was a statistically significant difference between the
groups. Extubation times were shorter in group 2 (group 1: 8.52
±
1.3 and group 2: 6.34
±
1.0 hours;
p
=
0.032).
While there were seven patients who had pleural effusions
requiring drainage in group 1, there were only two patients with
pleural effusions requiring drainage in group 2 (
p
=
0.044).
Whereas there were 14 patients with post-operative atrial
fibrillation (PAF) in group 1, the number of patients with PAF
was five in group 2 (
p
=
0.031). All PAF patients excluding
two were converted medically (amiodarone) to sinus rhythm in
group 1. The remaining two were converted to sinus rhythm by
D/C cardioversion. In group 2 all five patients with PAF were
converted to sinus rhythm medically.
The number of patients who needed pharmacological inotropic
support was 12 in group 1 and five in group 2. Pulmonary
infections such as pneumonia were more frequent in group 1
compared to group 2. There were no sternal infections or sternal
dehiscence in either group. The duration of ICU and hospital
stay was shorter in group 2. Post-operative data of the patients
are detailed in Table 2.
Discussion
CABG is a safe and effective surgical treatment that is performed
successfully in a wide variety of patients.
1
Nowadays the profile
of patients undergoing CABG is changing to a higher-risk
profile; elderly patients with co-morbid medical problems.
With improved experience, cardiac risk factors such as left
main coronary artery disease and angina class have lost their
predictive value for mortality in favour of extra-cardiac factors
such as peripheral vasculopathy, chronic renal failure or COPD.
6,7
The impact of COPD in patients undergoing open-heart
surgery is potentially problematic because of the additional
influence of CPB and median sternotomy.
8
It is well known that
CPB interferes with pulmonary function. CPB can also induce
adverse effects on alveolar stability by activating the complement
system, sequestration of neutrophils in the pulmonary vascular
bed, releasing oxygen-derived free radicals and changing the
composition of alveolar surfactant.
8
Atelectasis is one of the
most important problems after CPB, especially in the early post-
operative period.
Median sternotomy also has a negative influence on
pulmonary function. Structural changes in the chest wall after
sternotomy are the cause of restrictive pulmonary dysfunction,
which can be prolonged for weeks after the operation. Lung
injury becomes more prominent after surgery in COPD patients.
Therefore COPD has been established as an important risk factor
for mortality in patients undergoing CABG.
7
Depending on the severity of the pulmonary dysfunction,
the morbidity and mortality of the procedure can be very high
and sometimes almost prohibitive. Therefore a correct diagnosis
and defining its severity is mandatory because it could allow
better planning strategies.
9
In high-risk patients, it is imperative
to institute vigorous pre-operative measures to improve the
respiratory status before the surgical procedure. The degree
of severity of these risk factors has an important prognostic
relevance and not the risk factor itself. Mild COPD is well
tolerated by CABG patients in comparison with moderate or
severe COPD. As indicated by Fuster
et al
.,
7
FEV
1
must be the
reference variable when a patient with COPD is considered
for CABG, as is the creatinine level for chronic renal failure
patients.
7
Morbidity due to COPD usually increases with age and
is higher in males than females.
10
In their study, Fuster
et al
.
7
reported that the mortality rate was 13% in patients over 75
years, while it was 7% in patients under 75 years. In our study,
the patient population was on average 65 years, which was
younger than Fuster’s patient population, and we had three
mortalities in group 1 and one in group 2.
Adverse respiratory system events such as respiratory failure
and pneumonia have traditionally been the leading cause of
post-operative complications.
11
COPD patients particularly are
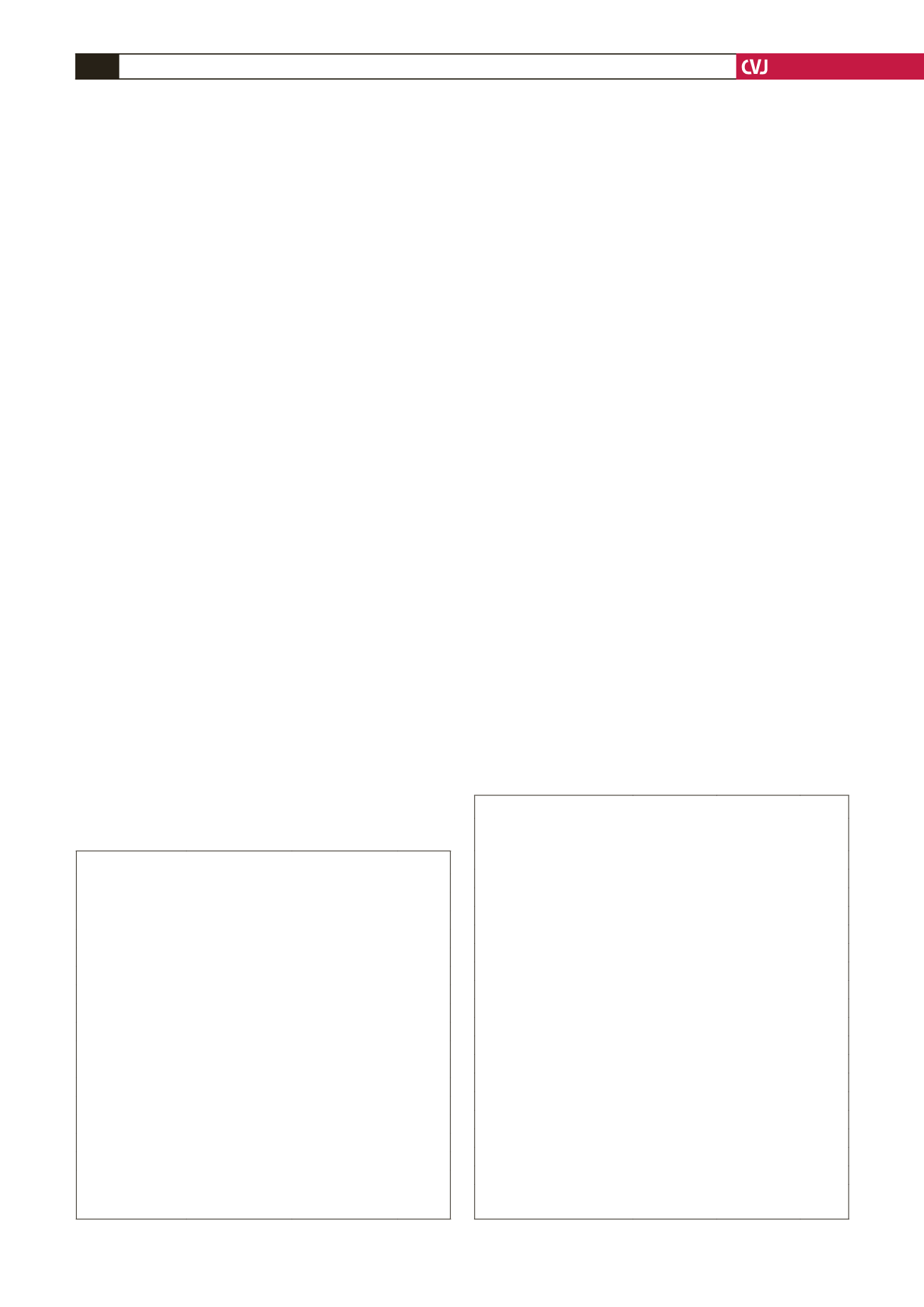
TABLE 1. PATIENT CHARACTERISTICS
Variable
Group 1 (
n
=
53)
Group 2 (
n
=
51)
p
-value
Age (years)
62.1
±
7.6
64.5
±
6.4
0.856
BMI
27.7
±
3.1
28.2
±
2.7
0.943
Gender
Male
39
38
0.842
Female
14
13
0.911
Hypertension
32
0.932
Diabetes
17
35
0.731
Renal disease
2
20
1
NYHA class
1.9
±
0.7
2
0.911
Mean FEV
1
(%)
46.1
±
2.3
2,0
±
0.8
0.823
EF (%)
53.3
±
11.5
48.2
±
2.1
0.678
Previous MI
23
50.2
±
10.8
0.956
Previous stroke
3
24
0.745
CRF
2
2
1
EuroSCORE
5.5
±
2.3
2
0.821
BMI: body mass index, NYHA: NewYork Heart Association, FEV:
forced expiratory volume, EF: ejection fraction, MI: myocardial infarc-
tion, CRF: chronic renal failure.
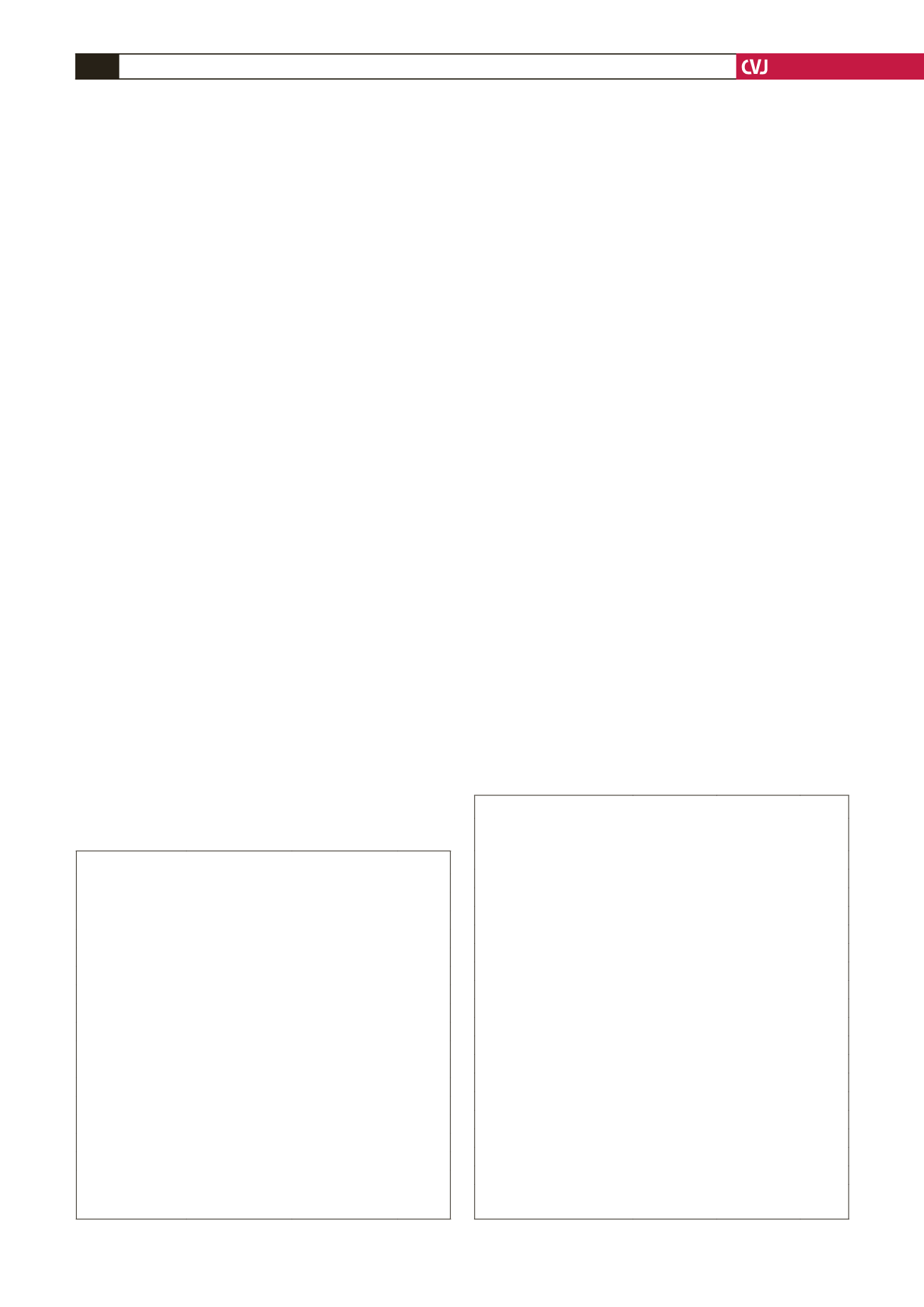
TABLE 2. POST-OPERATIVEVARIABLES OF THE PATIENTS
Variable
Group 1
(
n
=
53)
Group 2
(
n
=
51)
p
-value
Cross-clamp time (min)
67.2
±
16.7 65.4
±
19.2 0.453
CPB time (min)
140.5
±
43.6 135.3
±
50.4 0.654
Average number of grafts
3.1
±
1.0
2.9
±
0.9 0.744
Extubation time (h)
8.52
±
1.3
6.34
±
1.0 0.032
Re-intubation
1
–
0.5
Sternal dehiscence
–
–
–
Wound infections
1
–
0.5
Pleural effusions
7
2
0.044
Pneumonia
4
1
0.171
Mediastinitis
–
–
–
Atrial fibrillation
14
5
0.031
Other rhythm disturbances
–
–
–
Inotropic support
12
5
0.029
IABP support
3
2
0.742
LCOS
–
–
–
Length of ICU stay (days)
2.4
±
1.2
1.4
±
1.1 0.039
Length of hospital stay (days)
12.95
±
2.4 8.29
±
1.7 0.028
30-day mortality
3
1
0.302
CPB: cardiopuolmonary bypass, IABP: intra-aortic balloon pump, LCOS:
low-cardiac output syndrome, ICU: intensive care unit.