CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 1, January/February 2016
AFRICA
41
Evaluation of the angiographic parameters in the PPCI and
TT groups revealed a higher number of patients with single-
vessel disease in the TT group. Triple-vessel disease was more
common in the PPCI group. The groups were similar in terms of
bifurcation lesion, left dominance, drug-eluting stent use, direct
stenting, coronary ectasia, thrombus aspiration and tirofiban
infusion. Similar balloons were used with regard to diameters
and lengths. Increased stent diameters (
p
=
0.015) and lengths
(0.005) were observed in the PPCI group (Table 4).
Discussion
The results of this study demonstrated similar levels of
improvement in RV function among patients managed with PCI
within three to 12 hours from TT, and those managed with PPCI
following RV-STEMI.
There are several conventional methods of assessing RV
systolic function that should be incorporated into a routine
echocardiographic assessment. These are FAC, TAPSE, RV-S
′
,
and MPI. It is strongly recommended that at least one of the
above quantitative measures be incorporated into the routine
echocardiographic examination. 2D-derived estimation of RV
ejection fraction is not recommended because of the heterogeneity
of methods and the numerous anatomical assumptions.
13
RV-FAC is one of the parameters recommended for the
assessment of systolic function. However, this technique is
dependent on imaging and the operator’s skill. Normal values
of RV-FAC are accepted as
>
35%.
13
RV-FAC has been shown
to correlate with RVEF in studies performed using magnetic
resonance imaging (MRI). Heart failure, sudden death, stroke
and pulmonary embolism have also been shown to predict
mortality.
13,19
In the present study, there was no difference between the
groups with regard to mean RV-FAC values obtained before PCI
and at the one-month follow up. Mean RV-FAC values observed
at the one-month follow up were significantly increased within
each group compared to the pre-PCI period.
Isovolumic acceleration (IVA) is considered a useful method
to evaluate RV systolic function.
20
However this method is
not without disadvantages. It is angle-dependent and may be
influenced by age and heart rate. The lower limit of pulse wave
with tissue Doppler was accepted as 2.2 m/s
2
, as per the guideline
recommendations.
13
In our study, there was no difference between the groups in
terms of pre-PCI RV-IVA. Although pre-PCI, RV-IVA levels
were low in the two groups, mean levels were improved to normal
at the one-month follow up in both groups. The difference
between the early period and the one-month follow up was
significant in each group.
MPI may be used for the assessment of global heart function.
21
It enables evaluation of both systolic and diastolic function.
Reduced ventricular systolic function shortens the ejection time,
leading to increased MPI. MPI
>
0.4 with pulse Doppler and
MPI
>
0.55 with tissue Doppler are considered direct indicators
of impaired RV function.
13
A normal MPI value is 0.28
±
0.04 for
the RV, and 039
±
0.05 for the LV.
22
In a study by Karakurt
et al
., patients who were managed
with PPCI following non-anterior STEMI were compared to
those who received TT alone, and similar mean RV-MPIs were
observed in both groups at 72 hours after the infarction.
23
In our
study, there was no difference between the groups in terms of
mean RV-MPI values observed before percutaneous intervention
and at the one-month follow up. However, the mean RV-MPI
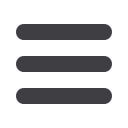
Table 3. Right ventricular systolic parameters according to
the echocardiographic evaluation periods
Parameter
PPCI
TT+PCI
Early period First month
p
-value Early period First month
p
-value
RV basal (mm) 37.3 (
±
4.4) 34.3 (
±
6.1) 0.042 37.9 (
±
5.1) 33.8 (
±
7.4) 0.018
RV mid (mm) 31.8 (
±
2.4) 26.9 (
±
3.6) 0.005 31.2 (
±
3.5) 27.5 (
±
2.8) 0.026
RV longitudi-
nal (mm)
72.2 (
±
5.4) 65.3 (
±
2.4) 0.038 73.1 (
±
2.4) 66.1 (
±
2.4) 0.032
RV-eDV
indexed (ml/m
2
)
64.3 (
±
9.4) 56.9 (
±
4.7) 0.006 63.2 (
±
5.6) 57.1 (
±
8.7) 0.012
RV-eSV
indexed (ml/m
2
)
37.1 (
±
4.3) 30.1 (
±
2.9) 0.008 38.6 (
±
3.9) 31.9 (
±
3.0) 0.017
RVEF (%)
43.1 (
±
8.3) 49.9 (
±
7.2)
<
0.001 42.6 (
±
8.8) 49.3 (
±
7.2)
<
0.001
RV-FAC (%)
29.9 (
±
7.4) 33.3 (
±
6.8) 0.011 29.4 (
±
7.4) 34.2 (
±
6.8) 0.006
RV-TAPSE
(mm)
16.1 (
±
4.0) 22.4 (
±
3.8)
<
0.001 16.7 (
±
4.2) 21.8 (
±
3.9)
<
0.001
RV-MPI
0.49 (
±
0.09) 0.41 (
±
0.12)
<
0.001 0.50 (
±
0.12) 0.40 (
±
0.14)
<
0.001
RV-IVA (m/s
2
) 2.24 (
±
0.64) 2.99 (
±
0.63)
<
0.001 2.31 (
±
0.52) 2.90 (
±
0.55)
<
0.001
RV-S
′
(cm/s)
9.1 (
±
2.2) 11.3 (
±
3.0)
<
0.001 9.5 (
±
1.1) 10.9 (
±
3.0) 0.003
RV apical
strain (%)
–9.7 (
±
1.8) –16.6 (
±
2.9)
<
0.001 –10.1 (
±
1.5) –15.9 (
±
2.1)
<
0.001
RV mid strain
(%)
–14.1 (
±
2.3) –22.6 (
±
3.6)
<
0.001 –14.9 (
±
1.9) –21.2 (
±
2.1)
<
0.001
RV basal strain
(%)
–18.2 (
±
4.7) –24.8 (
±
4.1) 0.006 –17.6 (
±
2.0) –24.2 (
±
2.1) 0.003
RV free strain
(%)
–14.0 (
±
2.7) –21.6 (
±
3.3)
<
0.001 –14.2 (
±
1.7) –21.1 (
±
3.7)
<
0.001
RV apical
strain rate (1/s)
–0.8 (
±
0.4) –1.5 (
±
0.5)
<
0.001 –0.9 (
±
0.3) –1.4 (
±
2.1) 0.004
RV mid strain
rate (1/s)
–1.1 (
±
0.6) –2.2 (
±
0.4)
<
0.001 –1.0 (
±
0.5) –2.1 (
±
2.1)
<
0.001
RV basal strain
rate (1/s)
–1.7 (
±
0.6) –2.3 (
±
0.5) 0.002 –1.6 (
±
0.4) –2.2 (
±
2.1)
<
0.001
RV free strain
rate (1/s)
–1.22 (
±
0.4) –2.11 (
±
0.4)
<
0.001 –1.29 (
±
0.5) –1.96 (
±
0.6)
<
0.001
LVEF (%)
49.3 (
±
8.3) 52.2 (
±
6.6) 0.048 48.4 (
±
7.6) 51.9 (
±
8.3) 0.040
LV-WMSI
1.48 (
±
0.27) 1.16 (
±
0.25)
<
0.001 1.52 (
±
0.34) 1.21 (
±
0.31)
<
0.001
eDV: end diastolic volume; EF: ejection fraction ; eSV: end-systolic volume; FAC:
fractional area change; IVA: isovolumic acceleration; LV: left ventricle; MPI: myocar-
dial performance index; RV: right ventricle; S
′
: tissue Doppler systolic wave; TAPSE:
tricuspid annulus planimetric systolic excursion; WMSI: wall motion score index.
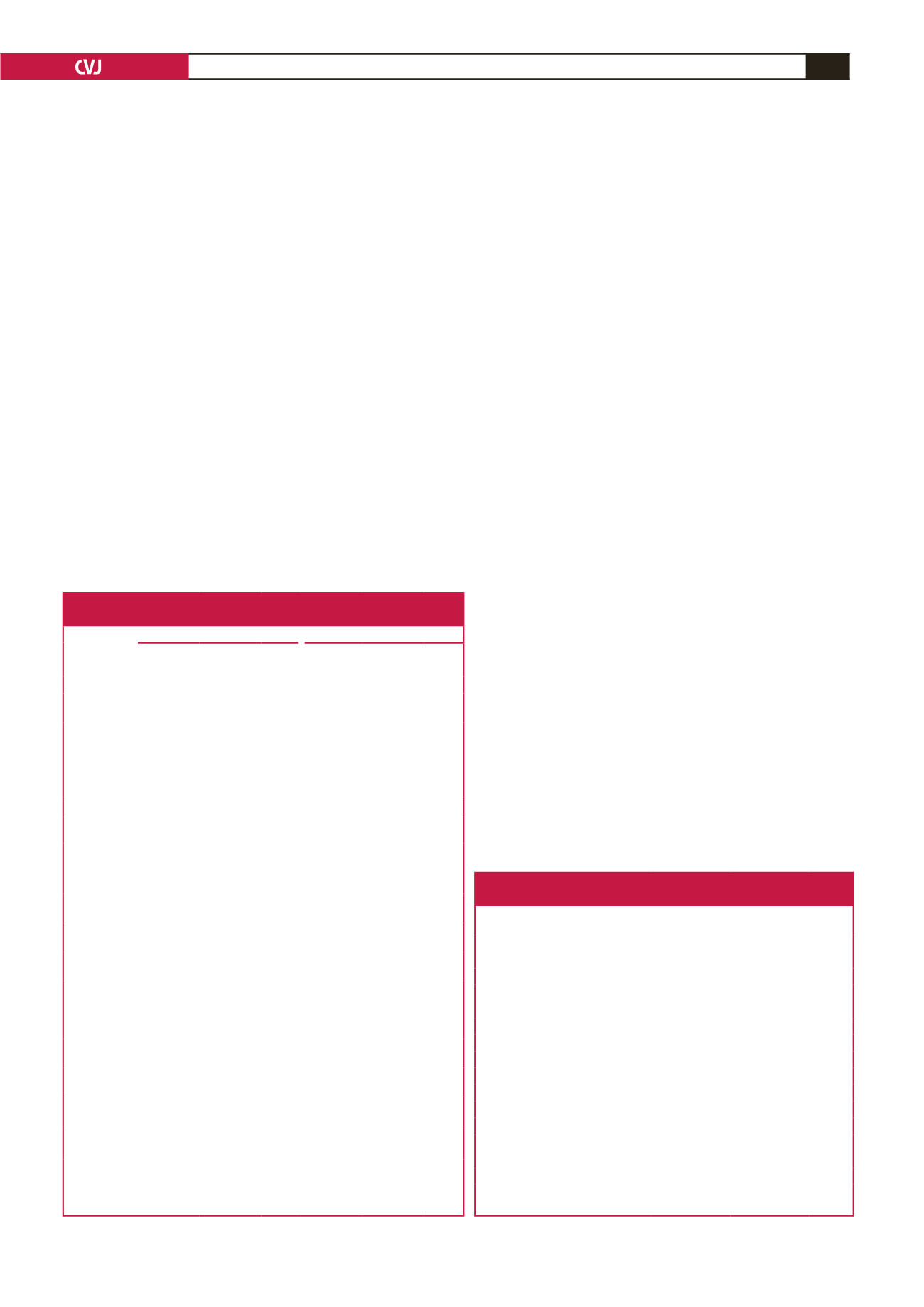
Table 4. Angiographic findings and coronary intervention
characteristics between the groups
PPCI
(
n
=
132)
TT+PCI
(
n
=
78)
p
-value
One-vessel coronary disease,
n
(%)
32 (24.2)
29 (37.2)
0.045
Two-vessel coronary disease,
n
(%)
52 (39.4)
31 (39.8)
0.820
Three-vessel coronary disease,
n
(%)
48 (36.4)
18 (23.1)
0.031
LMCA stenosis,
n
(%)
10 (7.5)
5 (6.4)
0.675
RCA proximal occlusion,
n
(%)
42 (31.8)
28 (35.9)
0.162
Thrombus aspiration,
n
(%)
13 (9.8)
6 (8.1)
0.443
Bifurcation lesion,
n
(%)
19 (14.4)
17 (23.0)
0.087
Left dominance,
n
(%)
9 (6.8)
8 (10.8)
0.285
Drug-eluting stents,
n
(%)
22 (16.7)
14 (19.2)
0.236
Direct stent implantation,
n
(%)
24 (18.2)
14 (19.2)
0.500
Coronary ectasia,
n
(%)
6 (4.5)
5 (6.4)
0.387
Balloon diameter (mm)
2.46
±
0.38
2.54
±
0.49 0.681
Balloon length (mm)
18.1
±
4.03
17.6
±
3.56 0.130
Stent diameter (mm)
3.18 (2.50–4.25) 2.96 (2.55–4.05) 0.015
Stent length (mm)
28.6 (14.5–38.5) 23.0 (15.3–34.8) 0.005
LMCA: left main coronary artery; PCI: percutaneous coronary intervention;
PPCI: primary percutaneous coronary intervention; TT: thrombolytic therapy.

















