
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
AFRICA
209
implant, and during long-term follow up.
1-8
Serial, non-invasive
echocardiographic studies would help management strategies of
these patients and identify mechanical dysfunction timeously.
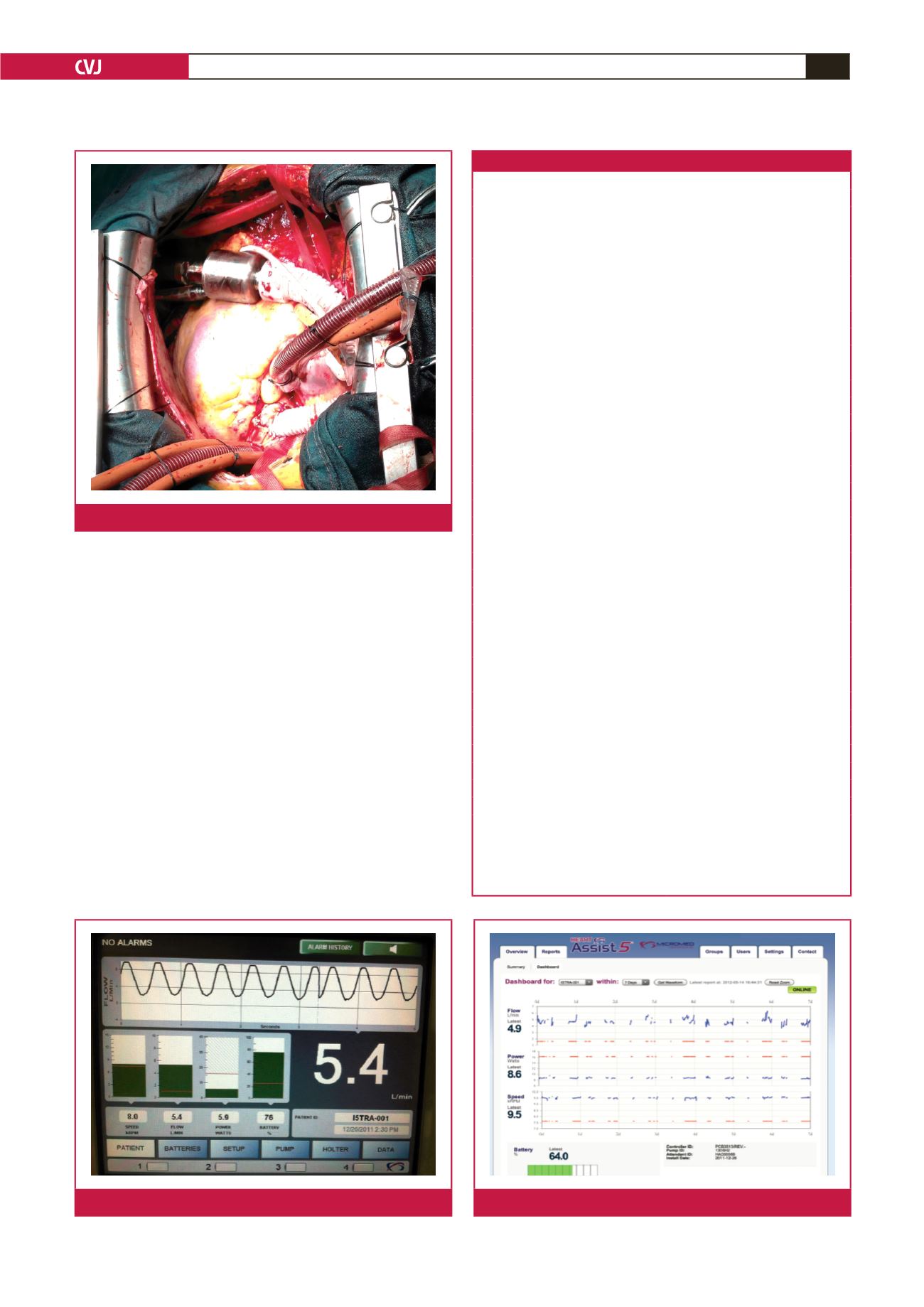
The Heart Assist 5 LVAD (Micromed Cardiovascular Inc,
Houston, TX) is small and compact, weighing 92 g and can
easily be implanted above the diaphragm (Fig. 1). The Heart
Assist 5 flow probe, an implantable ultrasonic flow, measures the
blood flow quite accurately while blood is pumped through the
outflow graft to the aorta. Changes in pump speed and electronic
current provide important information about the volume of
blood in the chambers and decompression of the heart, and
thus minor and major side effects can easily be detected. Also
remote monitoring of these patients helps with patient care, as
the primary physicians are informed either by cellphone message
or e-mail notification about marginal haemodynamic changes in
LVAD parameters (Figs 2, 3).
Although extensive data have been reported in the literature
concerning echocardiographic evaluation of other continuous-
flow pumps, there are no data on the Heart Assist 5 LVAD and
Fig. 1.
Heart Assist 5 LVAD implantation.
Table 1. Demographic and pre-implant characteristics
Parameters
Number of patients and mean
±
SD
Gender
Men
5
Women
4
Age, years
52
±
13
Weight, kg
74
±
12
Body surface area, m²
1.8
±
0.2
Heart disease
Ischaemic cardiomyopathy
8
Adriamycin-induced cardiomyopathy
1
Purpose of LVAD
Bridge to transplantation
9
Diabetes mellitus
3
Hypertension
3
AICD-CRT-D implantation
9
Previous cardiac surgery
CABG
1
Pre-implant support
Intra-aortic balloon pump
1
Haemodynamic values
Left ventricular ejection fraction, %
23
±
5
Cardiac index, l/min/m
2
2.04
±
0.4
Cardiac output, l/min
3.8
±
0.7
PCWP, mmHg
30
±
8
Coagulation profile
Prothrombin time, sec
17.3
±
7.5
International normalised ratio
1.58
±
0.6
Partial thromboplastin time, sec
33.9
±
2.8
Laboratory data
BUN, mg/dl
22
±
10
Creatinine, mg/dl
1.17
±
0.3
Na, mEq/l
136
±
2
Albumin, g/l
3.8
±
0.5
Alkaline phosphatase, U/l
73
±
25
SGOT, U/l
18
±
10
SGPT, U/l
26
±
23
Total bilirubin, mg/dl
0.92
±
0.5
SD = standard deviation; LVAD = left ventricular assist device; AICD = auto-
matic implantable cardioverter defibrillator; CRT-D = cardiac resynchronisation
therapy device; CABG = coronary artery bypass grafting; PCWP = pulmonary
capillary wedge pressure; BUN = blood urea nitrogen; Na = sodium; SGOT
= serum glutamic oxaloacetic transaminase; SGPT = serum glutamic pyruvic
transaminase.
Fig. 2.
Heart Attendant, the portable console.
Fig. 3.
Remote monitoring of Heart Assist 5.

















