
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
AFRICA
211
velocity was 0.9
±
0.2 (0.8–1.2) m/s, and aortic valve opening was
observed every one-to-one cycle or one-to-three cycle.
Since eight patients had ischaemic cardiomyopathy and
one had had coronary artery bypass grafting (CABG) 10
years earlier, remission of their end-stage heart failure was
not expected. All our patients had had automated internal
cardioverter defibrillator (AICD) and cardiac resynchronisation
therapy (CRT-D) implantation prior to the LVAD implantation.
One patient had a ventricular fibrillation (VF) event in the ward
and had cardiopulmonary resuscitation. He had his AICD-
CRT-D implanted prior to the LVAD surgery. Two patients
had experienced ventricular tachycardia (VT) at home due to
dehydration during the summer, and their AICD had been
interrupted during the attacks.
There were a few hospitalisations because of minor
complications. One patient complained of a coffee-grinding
noise coming from his pump three months post-implant, and
the remote monitoring system also documented frequent excess
current alarms and increased power at different hours of the day.
The patient was hospitalised for possible thrombus formation
or device malfunction. The data were analysed at Micromed
Cardiovascular Inc, Houston, Texas. The coagulation profile was
in the normal range for a LVAD patient, his INR was 3.2, and
his lactate dehydrogenase level was 606 U/l, which was gradually
elevated up to 120 days after LVAD implantation.
Serial echocardiographic studies were done weekly to rule out
possible thrombus formation in the left ventricle, the orifice of
the inflow cannula, outflow conduit and aortic valve cusps. The
patient received heparin infusion with close monitoring of his
coagulation profile. There was no absolute finding in the echo
studies to confirm thrombus formation or determine the reason
for the coffee-grinding noise, since we were not able to visualise
the titanium impeller. We guessed that there may have been a
blood clot there, which caused the increased power. The noise
stopped after the fifth day of heparin infusion.
A female patient had uncontrolled diabetes, she had gradually
gained 7 kg by the sixth month post-operatively, and suffered
from recurrent urinary tract infections. She was admitted with
fever, tachycardia, post-diabetic ketoacidosis and documented
urinary tract infection. Her echocardiographic study was done
in a sub-optimal position due to her tachycardia. She received
anti-arrhythmic and antibiotic regimens, and a few days later she
was in sinus rhythm, her heart rate was 89–95 beats per minute,
and her fever was gone. Her echo studies were repeated and
LVAD optimisation was done. She was discharged from hospital
with 9 500 rpm, her CO was 4.7 l/min and the pulsality index
was 2.31 m/s.
Four patients were followed up for more than two years, and
two for more than a year. Three patients died due to multi-organ
failure. One international patient had heart transplantation in
the Republic of China. The longest supported patient was for
more than three years, with a good quality of life.
Discussion
All data for each patient had been collected in each portable
console, Heart Attendant (Micromed Cardiovascular Inc,
Houston, TX), so with the universal serial bus (usb) connection,
all the data could be downloaded and could be easily analysed.
Online connection of the Heart Attendant to the internet assists
in patient care and provides 24 hours a day, seven days a week
monitoring of the LVAD patient. This technology decreases
hospital admissions for each alarm detection, as the clinicians
can track the patient with the remote monitoring system and
help him/her by phone.
This technology differentiates Heart Assist 5 LVAD from
other continuous-flow pumps. The implantable flow probe
also helps to assess even minor dehydration problems, which
can be solved without admission to hospital. We experienced
low-flow alarms during the summer months and suggested our
patients take in extra fluid during summer.
15
Fine-tuning of
the Heart Assist 5 LVAD with the implantable flow probe and
portable console was convenient, and the LVAD speed change
echo studies enabled easy optimisation of the device during
in-hospital echocardiographic studies.
There are reports of large single-centre echocardiographic
studies of other continuous-flow and centrifugal pumps in the
literature.
8-13
These pumps have been approved by the United
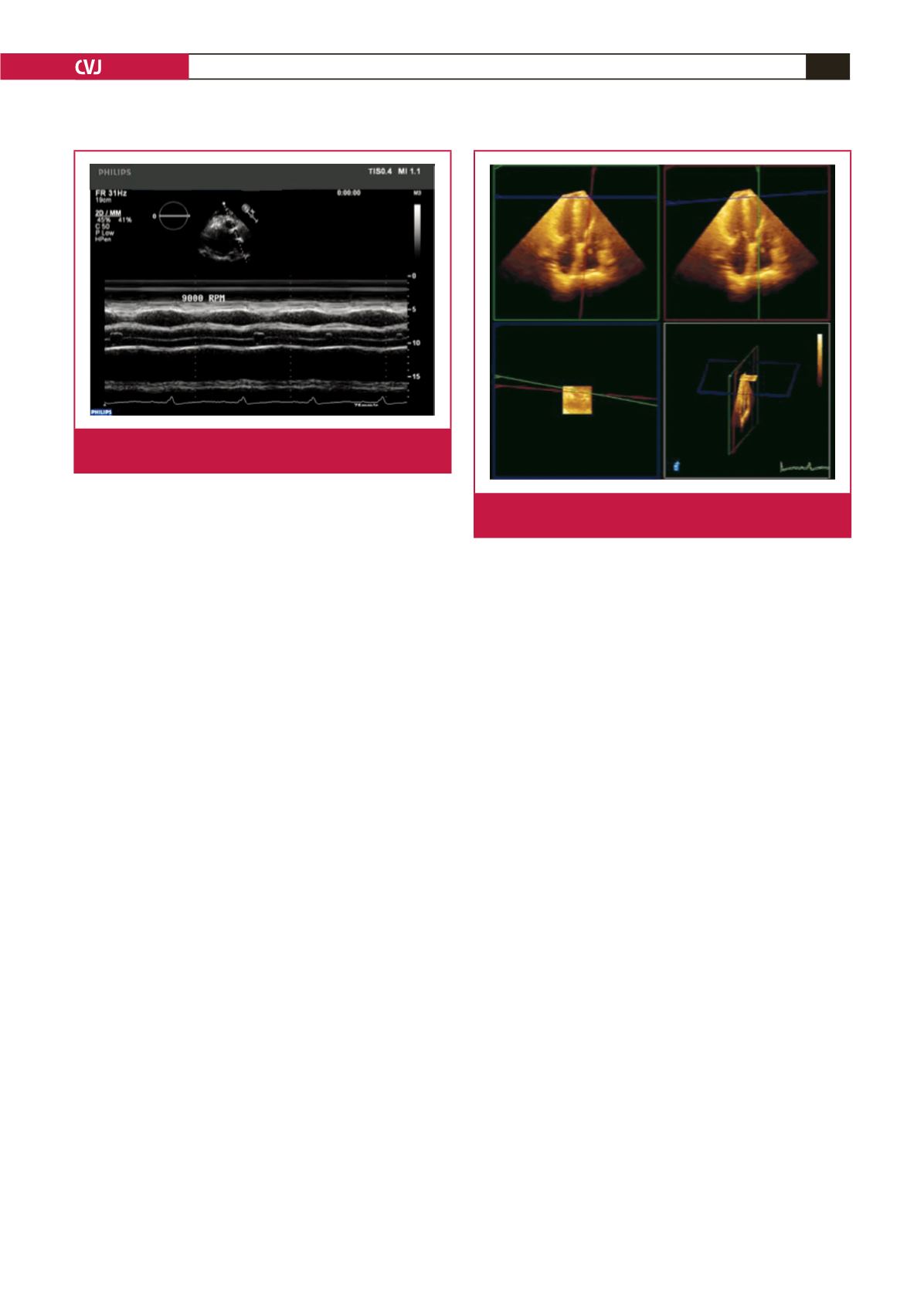
Fig. 5.
Evaluation of aortic valve opening times with M mode
TTE.
Fig 6.
Left ventricular inflow cannula visualisation with 3D
TTE.

















