
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
134
AFRICA
Case Report
Pacemaker syndrome with sub-acute left ventricular
systolic dysfunction in a patient with a dual-chamber
pacemaker: consequence of lead switch at the header
Mohammad Reeaze Khurwolah, Brian Zwelethini Vezi
Abstract
In the daily practice of pacemaker insertion, the occurrence
of atrial and ventricular lead switch at the pacemaker box
header is a rare and unintentional phenomenon, with less
than five cases reported in the literature. The lead switch
may have dire consequences, depending on the indication
for the pacemaker. One of these consequences is pace-
maker syndrome, in which the normal sequence of atrial and
ventricular activation is impaired, leading to sub-optimal
ventricular filling and cardiac output. It is important for the
attending physician to recognise any worsening of symptoms
in a patient who has recently had a permanent pacemaker
inserted. In the case of a dual-chamber pacemaker, switching
of the atrial and ventricular leads at the pacemaker box head-
er should be strongly suspected. We present an unusual case
of pacemaker syndrome and right ventricular-only pacing-
induced left ventricular systolic dysfunction in a patient with
a dual-chamber pacemaker.
Keywords:
permanent pacemaker, lead switch, pacemaker
syndrome, right ventricular-only pacing-induced left ventricular
systolic dysfunction
Submitted 27/5/14, accepted 14/9/16
Cardiovasc J Afr
2017; 28: 134–136
www.cvja.co.zaDOI: 10.5830/CVJA-2016-081
In the daily practice of pacemaker insertion, the occurrence of
atrial and ventricular lead switch at the pacemaker box header is
a rare and unintentional phenomenon, with less than five cases
reported in the literature.
1
The diagnosis of lead switch at the
header is usually straightforward and is noticed quite early. If
not, the possibility of this important complication should be
considered in any patient presenting with ill-defined symptoms
during pacemaker follow up.
Patients may present with a variety of symptoms, depending
on the underlying rhythm, pacing rate and percentage of
the paced beats. The symptoms of pacemaker syndrome are
usually non-specific but often include dizzy spells, shortness of
breath, fatigue, near-syncope, syncope or frank heart failure.
The occurrence of right ventricular-only pacing-induced left
ventricular systolic dysfunction has been well documented.
2-4
Case report
A 40-year-old man presented with symptoms of undue fatigue
and shortness of breath with minimal exertion. His resting heart
rate was noted to reach 28 beats per minute (bpm) during waking
hours. He was diagnosed with sick sinus syndrome and had a
dual-chamber permanent pacemaker inserted. Subsequently,
he reported feeling more ill and complained of dizziness, near-
syncope and syncope, worsening of shortness of breath, more
fatigue, and what he described as a ‘strange heartbeat with
fluttering’. Prior to the dual-chamber pacemaker insertion, he
had undergone coronary angiography and left ventriculography,
which showed normal epicardial coronary arteries and a left
ventricular ejection fraction (LVEF) of 74%.
On physical examination post pacemaker insertion, his blood
pressure was 106/76 mmHg, with a heart rate (HR) of 76 bpm.
The jugular venous pressure was elevated up to the angle of
the jaw and cannon waves were present. His heart sounds were
otherwise normal with no murmurs elicited, and there were no
signs of heart failure. His chest was clear. The electrocardiogram
Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-
Natal, South Africa
Mohammad Reeaze Khurwolah, MB ChB (UCT), nush.11426@
hotmail.comBrian Zwelethini Vezi, FCP (SA)
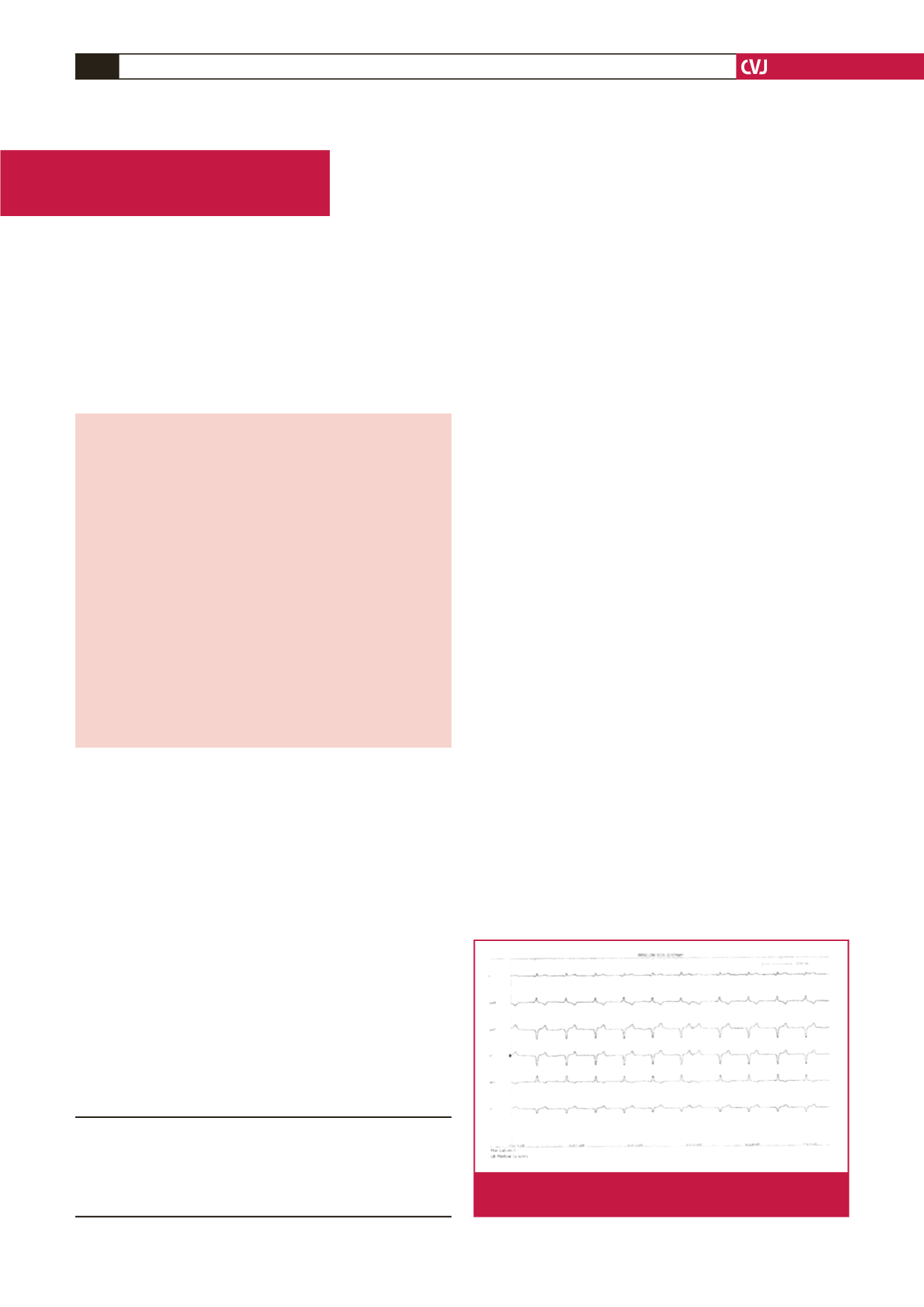
Fig. 1.
Paced QRS with sensed P wave at the end of the
QRS, indicative of atrioventricular dyssynchrony.

















