
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
AFRICA
267
The discrepancy between best practice (based on high-
quality evidence) and the care provided in routine clinical
practice is called the ‘care gap’. This includes situations in
which interventions with proven efficacy are under-utilised. This
description is most marked in Africa, where it is favoured by
poverty and inadequate utilisation of existing resources. Despite
strong evidence of the management benefit, this can reflect as
poor awareness and control of CVD rates or risk factors.
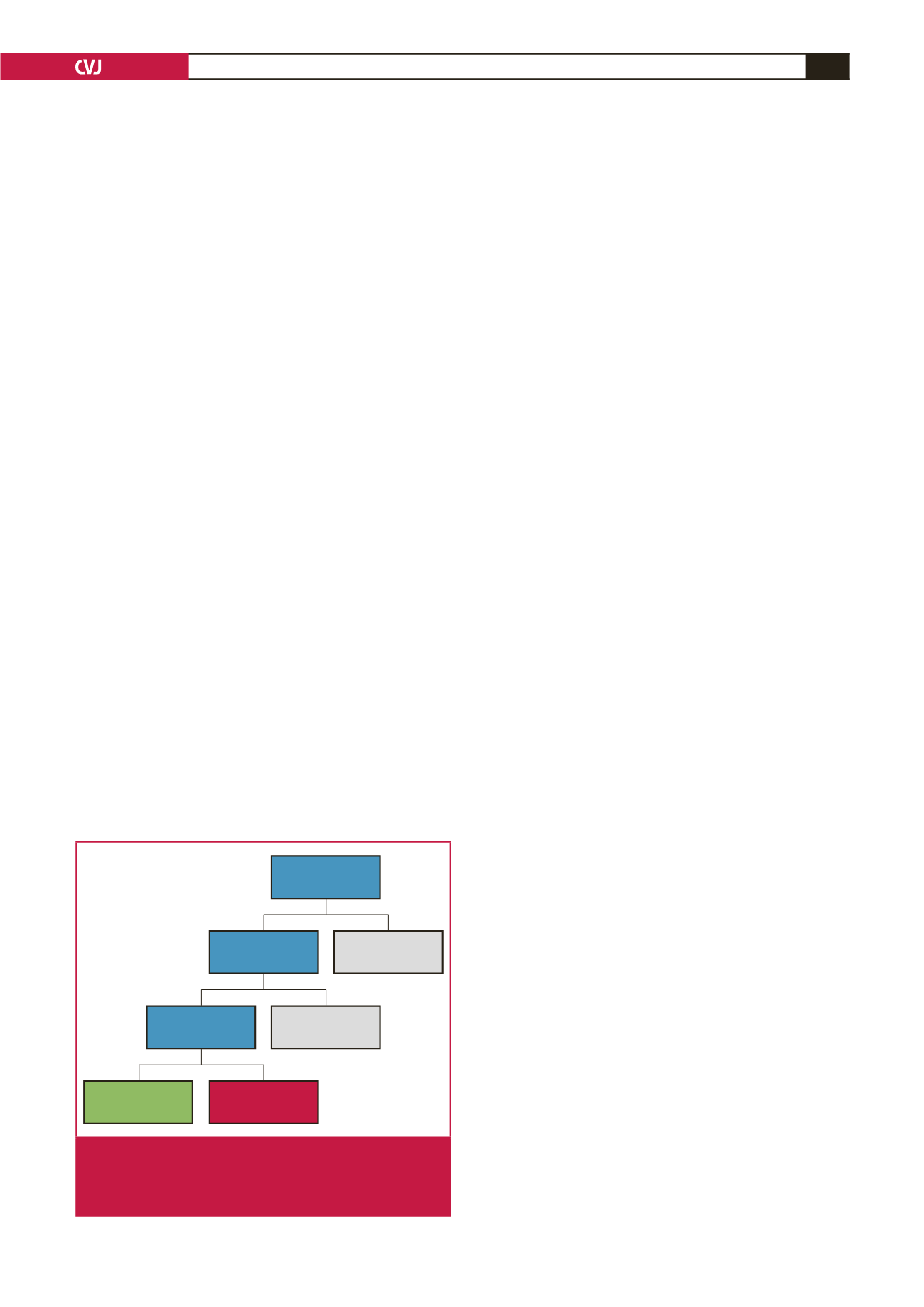
Current data on awareness and hypertension control rates in
SSA are from a wide range of studies differing in methodology
and limiting the opportunity for reliable comparisons. However,
available data show that the high prevalence of hypertension in
Africa, as in other LMICs, is coupled with low awareness and
control rates (Fig. 3), a reflection of a maximal care gap.
5-8
In 2011, UN member states acknowledged at the highest
international level that premature deaths from NCDs reduce
productivity and curtail economic growth, causing significant
social challenges in most countries.
9
In 2015, the previous target of
25% reduction in rate of premature mortality from NCDs by 2025
was extended to a reduction of 33% by 2030, through prevention,
treatment and promotion of mental health and wellbeing.
10
Since 2004, the African Union, in a pro-active approach,
named hypertension one of the continent’s greatest health
challenges after HIV/AIDS. After more than a decade, this
political enthusiasm, which is crucial for the development and
implementation of any healthcare policy, has yet to be translated
into public health action. The role of hypertension experts is key
to facilitate the states’ action to adequately contain this threat.
In a simple and practical hypertension policy, the PASCAR
approach emphasises working in collaboration with all other
stakeholders to set clear goals and define priority actions and
minimum standards of African healthcare systems.
The World Heart Federation roadmap and
other relevant initiatives
As part of the WHO’s target in reducing heart attacks and
stroke by 2025, the World Heart Federation (WHF) launched a
roadmap focusing on raised BP during the 2015 World Health
Assembly in Geneva.
11
Herein the routes are described towards
reducing premature cardiovascular mortality rate by 25%,
11
focusing on presenting practical steps for hypertension control.
For effective hypertension control, four population groups were
identified: people who are unaware of their BP status; those who
are aware of having raised BP but it is uncontrolled; those who
are aware of their raised BP, which is under control; and those
who are aware of having normal BP.
After identifying the target population, practical steps are
provided for improving hypertension management. These include
opportunistic screening for awareness of BP status and effective
drug treatment for high BP.
The use of generic antihypertensive medications rather than
proprietary medications is encouraged, to substantially reduce
the cost of care, but with a caveat for the need to ensure
quality generic medications. Bearing in mind the holistic nature
of healthcare delivery, this initiative identified health-system
requirements to achieve BP management targets and include
human, physical and intellectual resources, healthcare delivery,
healthcare recipients, financing, and governance and information
systems.
With global information technology tools available, the
suggestion of using e-health, particularly m-health, for patient
education is a very feasible approach in the guidelines. If
well applied, this could be a useful tool in hypertension
control. This roadmap is anticipated to substantially bridge
the gap between HIC and LMIC in terms of hypertension
management and control policy. The WHO Package of
Essential Non-communicable (PEN) Disease Interventions for
Primary Healthcare in Low-Resource Settings is an integrated
approach to NCDs focusing exclusively on primary healthcare
in low-resource settings.
12
The WHF roadmap provides a global framework to reduce
CVD mortality, focusing on evidence-based interventions.
Strong emphasis is placed on health systems, cost-effectiveness
and subsequent evaluation of programmes. Hypertension as a
single risk factor, and an entry point to prevent CVD rather than
the absolute-risk approach, provides a framework to identify
roadblocks in implementing evidence-based interventions.
Hypertension seldom occurs in isolation, co-existing with other
CVD risk factors, contributing to the absolute-risk status.
The PASCAR roadmap strongly emphasises hypertension as a
global health crisis and major threat. We hope that hypertension
screening will increase in the next eight years, resulting in a
paradoxical increase in the prevalence of hypertension. For this
reason, the task force’s target is to increase treatment and control
rates among the treated subjects by 25% in the SSA region by 2025.
We identified roadblocks to the control of hypertension in
the African region and proposed solutions to these roadblocks,
thus defining the best strategy to achieve this in SSA. Because
the epidemic of NCDs is driven by globalisation, urbanisation,
demographic trends and socio-economic conditions,
13
interventions to reach our targets are required from the health
sector and other governmental sectors, along with civil society
and the private sector.
Therefore, guidance is provided for policy makers, healthcare
professionals (nurses, general practitioners, family doctors,
internists, cardiologists, nephrologists and other hypertension
specialists), patients, the private sector and the public, including
Prevalence 30%
(27–34%)
Awareness 27%
(7–56%)
Not aware
73%
Treated 18%
(14–22%)
Untreated
82%
Controlled* 7%
(5–8%)
Uncontrolled
93%
*BP
<
140/90 mmHg
Fig. 3.
Prevalence, awareness, treatment and control of
hypertension in Africa. Numbers are from Ataklte
et al
.
Burden of undiagnosed hypertension in sub-Saharan
Africa: A systematic review and meta-analysis.
5

















