
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
264
AFRICA
4. Annually monitor and report the detection, treatment and
control rates of hypertension, with a clear target of improve-
ment by 2025, using the WHO STEPwise surveillance in all
countries.
5. Integrate hypertension detection, treatment and control
within existing health services, such as vertical programmes
(e.g. HIV, TB).
6. Promote a task-sharing approach with adequately trained
community health workers (shift-paradigm).
7. Ensure the availability of essential equipment and medicines
for managing hypertension at all levels of care.
8. Provide universal access and coverage for detecting, treating
and controlling hypertension.
9. Support high-quality research to produce evidence that will
guide interventions.
10. Invest in population-level interventions for preventing hyper-
tension, such as reducing high levels of salt intake and
obesity, increasing fruit and vegetable intake and promoting
physical activity.
African ministries of health, in their leadership roles, are called
to adopt the 10-point action plan and customise it at a country
level using a multi-sectoral approach. PASCAR calls on NGOs,
all fraternal organisations, healthcare leaders and other members
of the international community to join in this ambitious
endeavour to support efforts by African ministries of health
in reducing the burden of hypertension in Africa. Effective
advocacy towards policy makers and politicians in national
governments is particularly encouraged.
Hypertension definitions
There is a graded relationship between blood pressure (BP)
levels, as low as 115/75 mmHg, and cardiovascular disease
(CVD) risk.
1
However, hypertension is defined as the BP level
above which treatments have been shown to reduce clinical
events in randomised trials, which is accepted as ≥ 140 mmHg
systolic and/or ≥ 90 mmHg diastolic BP. The classification of
BP levels used for defining hypertension is presented in Table 1.
Hypertension burden in Africa
Hypertension has progressively become a major threat to the
well-being of people in sub-Saharan Africa (SSA). During the
past four decades, the highest levels of BP worldwide have shifted
from high-income countries (HIC) to low- and middle-income
countries (LMIC) in South Asia and SSA.
2
The WHO estimates
that the prevalence of hypertension is highest in the African
region, with about 46% of adults aged 25 years and older being
hypertensive.
3
This compares to 35% in the Americas and other
HIC and 40% elsewhere in the world.
3
High hypertension rates, ranging from 19.3% in Eritrea to
39.6% in the Seychelles, were reported for 20 African countries
in WHO STEPS (STEPwise approach to surveillance) surveys
conducted between 2003 and 2009.
4
In a systematic review, the
pooled prevalence in over 110 414 participants aged ± 40 years
in 33 surveys was 30% (95% confidence interval: 27–34%).
5
In
Table 1. Definitions of classes of raised blood pressure
Category
SBP (mmHg)
DBP (mmHg)
Optimal
< 120
< 80
Normal
120–129
80–84
High normal
130–139
or
85–89
Grade 1 hypertension (mild)
140–159
or
90–99
Grade 2 hypertension (moderate)
160–179
or
100–109
Grade 3 hypertension (severe)
≥ 180
or
≥ 110
Isolated systolic hypertension
≥ 140
and
< 90
SBP, systolic blood pressure; DBP, diastolic blood pressure
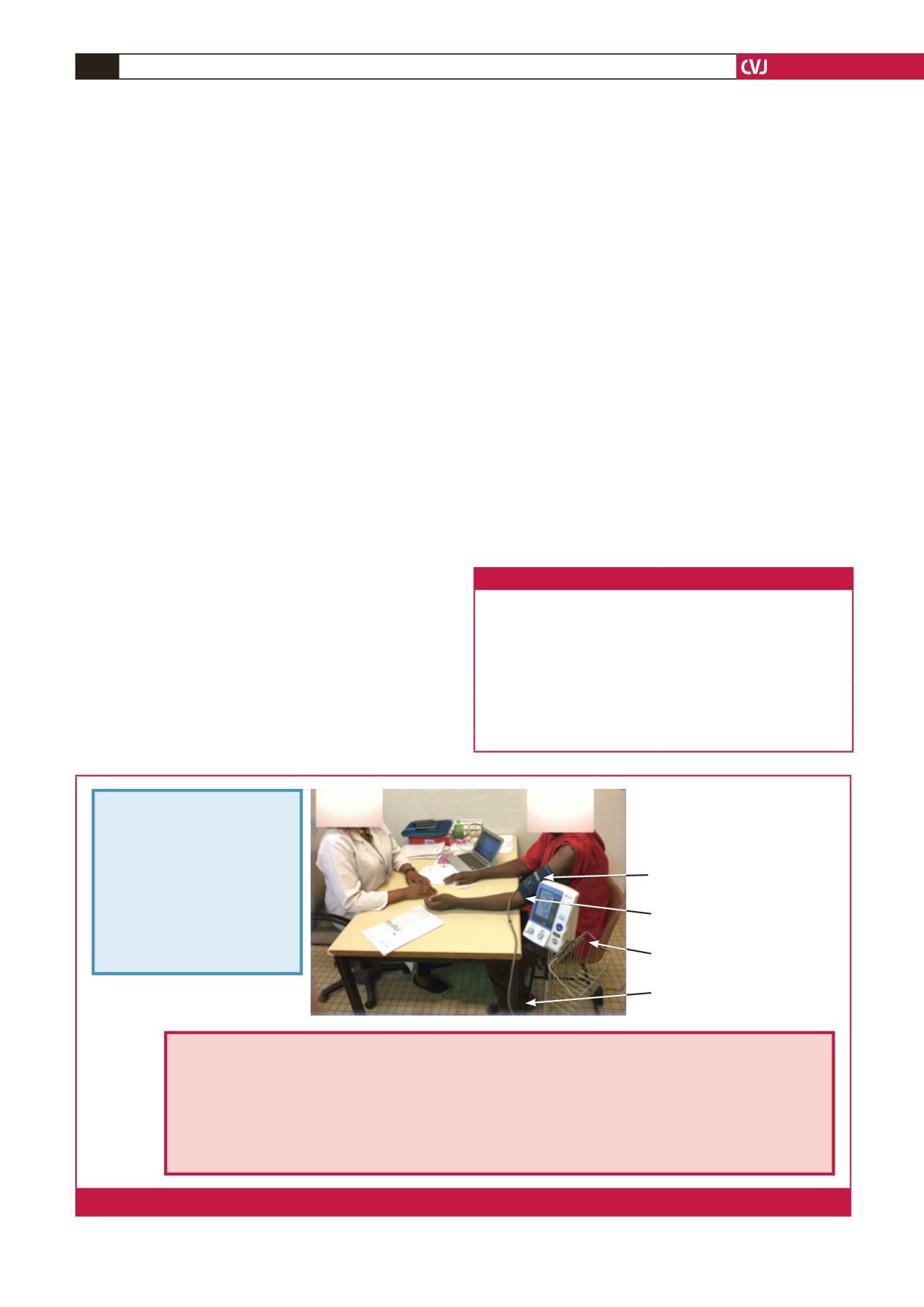
Arm supported at
the level of the heart
Do not speak during
the measurement
Put cuff on bare arm,
3 cm above the elbow
Be seated, with back
supported by the chair
BP measurement
• Prepare the patient
• Choose the appropriate cuff size
• Place the cuff and check that the tightness of the cuff is appropriate
• Press the start button
• The cuff will inflate and deflate, at the end of the measurement systolic, diastolic BP and pulse rate will be displayed
• Record the reading, then deflate the cuff
• Repeat the measurement after 1 minute
• Take two readings and obtain the average
Legs uncrossed
Feet supported by the ground
Patient preparation
• No caffeine, smoking or alcohol
for preceding 30 minutes
• A quiet warm setting is required
• Bladder and bowel should be
emptied
• No exogenous adrenergic
stimulatns e.g. nasal
decongestants or eye drops for
papillary dilation
• Patient should be calmly seated
for 5 minutes
If ausculatory method is used, more info
on technique can be sought at https://www.
youtube.com/watch?v=-LqKmrmaHskFig. 1.
PASCAR recommendations for blood pressure measurement, thresholds and action required following appropriate office measurement.

















