
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
AFRICA
e3
formation of a fistula between the aneurysm and right atrium.
2
A
ruptured sinus of Valsalva aneurysm is by far the most common
cause of aorta–right atrial tunnel.
3
Aneurysms of the sinus of Valsalva were first described by
Thurman in 1840 and remain relatively rare.
1
The incidence of
aneurysm of the sinus of Valsalva is reported to range between
0.1 and 3.5% of all congenital cardiac anomalies. Acquired
sinus of Valsalva aneurysms occur less frequently and causative
factors include degenerative diseases (atherosclerosis, connective
tissue disorders and cystic media necrosis), infections (syphilis,
bacterial or fungal endocarditis and tuberculosis), or thoracic
trauma.
4
The aetiopathogenesis of congenital aneurysms is poorly
understood.
5
The right coronary sinus and the non-coronary
sinus arise embryologically from the fusion of the bulbar septum
and truncal ridges. Incomplete fusion can result in aneurysm
formation within the septum when subjected to long-standing
systemic arterial pressure (left-to-right shunt).
6
Weakening of the
aortic wall leads to rupture and the establishment of a fistulous
tract that may communicate with any of the cardiac chambers,
the right atrium being the most common.
3
This is also closely
related to membranous ventricular septum. Ventricular septal
defects occur simultaneously in approximately 40% of patients
with congenital aneurysms.
4
The frequency of ruptured sinus of Valsalva aneurysm varies
according to the location: 60% in the right sinus, 42% in the
non-coronary sinus and only 10% in the left sinus.
7
Aorta–right atrial tunnel can be classified according to the
origin and course in relation to the ascending aorta, therefore
termed anterior or posterior.
8
Sakakibara and Konno
10
proposed
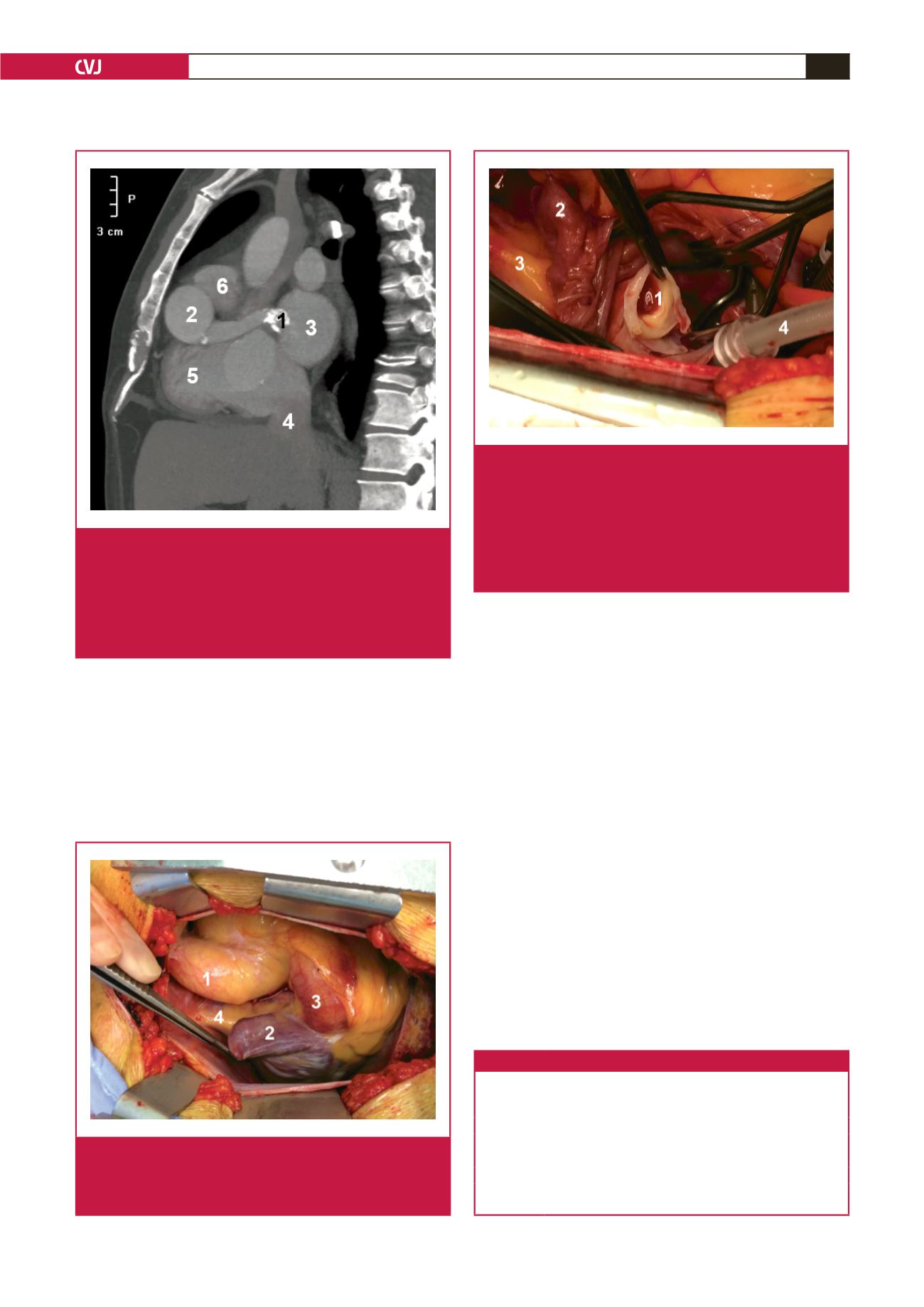
Fig. 5.
CT angiogram oblique sagittal image. 1, distal end of
tunnel; 2, proximal end of tunnel; 3, left atrium; 4, infe-
rior vena cava; 5, right ventricle; 6, pulmonary trunk; 7,
descending aorta. There is a small dense calcification
at the origin of the tunnel and dense mural calcifica-
tions at the distal end of the tunnel. The tunnel is long,
tortuous and dilated.
Fig. 6.
Intra-operative image. The right atrial appendage has
been retracted and the tunnel is demonstrated origi-
nating from the proximal aorta. 1, aorta; 2, right atrial
appendage; 3, tunnel; 4, superior vena cava.
Fig. 7.
Intra-operative image. Right atrium is opened and
the windsock excised. The distal end of the tunnel
is demonstrated opening into the right atrium with a
thick collagenised wall due to the high pressure of the
shunt. 1, distal end of the tunnel, the opening is within
the right atrium; 2, right atrial appendage, which has
been retracted; 3, superior vena cava; 4, retrograde
cardioplegia cannula.
Table 1. Classification for SVA proposed by Sakakibara and Konno
9
Type I
Connect the right SV and the existing tract of the RV below the
pulmonary valve
Type II
Connect the right SV and the VD in the supra ventricular crest
Type IIIa
Connect the right SV and the RA
Type IIIv
Connect the posterior zone of the right SV and the RV
Type IIIa + v Connect the right SV and both the RA and RV
Type IV Connect the non-coronary SV and the RA
SVA, sinus of Valsalva aneurysm; SV, sinus of Valsalva; RV, right ventricle; RA,
right atrium.

















