
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
AFRICA
e7
On physical examination, his blood pressure was
132/68 mmHg, heart rate was regular at 82 beats/min and
electrocardiography was normal. Chest auscultation was
normal but a chest X-ray revealed mediastinal widening and
cardiomegaly. His family history was unremarkable.
Transthoracic echocardiography (TTE) showed the presence
of a mechanical aortic valve prosthesis in its normal anatomical
position with normal function, excess dilatation of the proximal
ascending aorta (132 mm) and normal left ventricular function. A
thoracic contrast-enhanced computed tomography (CT) imaging
study revealed a 132.5-mm non-ruptured giant aneurysm and
an intra-luminal flap image confined to the ascending aorta (De
Bakey type II) that was consistent with dissection (Fig. 1B–D).
Surprisingly, despite a normal aortic arch and branches, there
was an aortic coarctation just distal to the subclavian artery
(Fig. 2A, D).
The patient was haemodynamically and clinically stable and
was admitted to our unit for surgery, which consisted of tubular
graft interposition in the supracoronary ascending aorta (Fig.
2B–D). He was weaned from mechanical ventilation nine hours
postoperatively, and was transferred to the ward on day two. He
was discharged uneventfully at day seven. A follow-up thoracic
CT at two months showed no problems, and the patient was
subsequently followed up in the out-patient unit (Figs 2C, D,
3A–D).
Surgical technique
As the wall of the ascending aorta was adjacent to the sternum
(Fig. 1B, D), arterial cannulation from the right axillary artery was
performed, as well as venous cannulation under transoesophageal
guidance, from the right femoral vein extending up to the
right atrium. Cardiopulmonary bypass (CPB) and cooling was
initiated. In such cases, CPB is instituted prior to resternotomy,
using deep hypothermia in the event that circulatory arrest is
required to gain control of the ascending aorta.
As expected, the aneurysmatic aortic wall adjacent to the
sternum was damaged during this procedure. In accordance with
the pre-planned surgical strategy, CPB was suspended and deep
hypothermia was used for a very short period of time (20°C),
during which the aneurysmal sac was rapidly dissected in the
distal direction and a clamp was placed at the origin of the aortic
arch, which had normal dimensions. CPB was then re-initiated.
Cardiac arrest with hypothermic blood cardioplegia was
achieved via hypothermic blood given into the right and left
coronary arteries using an osteal cannula, and myocardial
protection was provided. Due to the adhesions, cardiac venting
was performed through the pulmonary artery. After the body
temperature was increased to 27°C, moderate hypothermic
circulatory arrest was attained, followed by antegrade selective
cerebral perfusion at a flow rate of 10 ml/kg. A selective cannula
was then placed into the left main carotid artery to provide
bilateral cerebral perfusion. Cranial oxygenation and perfusion
were monitored using near-infra-red spectroscopy (NIRS).
After ensuring cerebral protection, a distal aortic anastomosis
was performed using no 32 Dacron tubular grafts with the
double-Teflon felt technique during moderate hypothermia. A
clamp was then placed on the Dacron graft and warming was
initiated. Without complete resection of the aneurysmatic aorta
from the supra-coronary region, the anastomosis of the proximal
aorta was completed with pledgeted 4/0 sutures in the lower half,
and the double-Teflon felt technique in the upper half.
After air evacuation and completion of warming, the patient
was gradually weaned off CPB. After bleeding was controlled,
the patient was de-cannulated and was transferred to the
intensive care unit.
Discussion
This case is of interest from several points of view. First is the
asymptomatic clinical course of a giant aneurysm of 13.25 cm
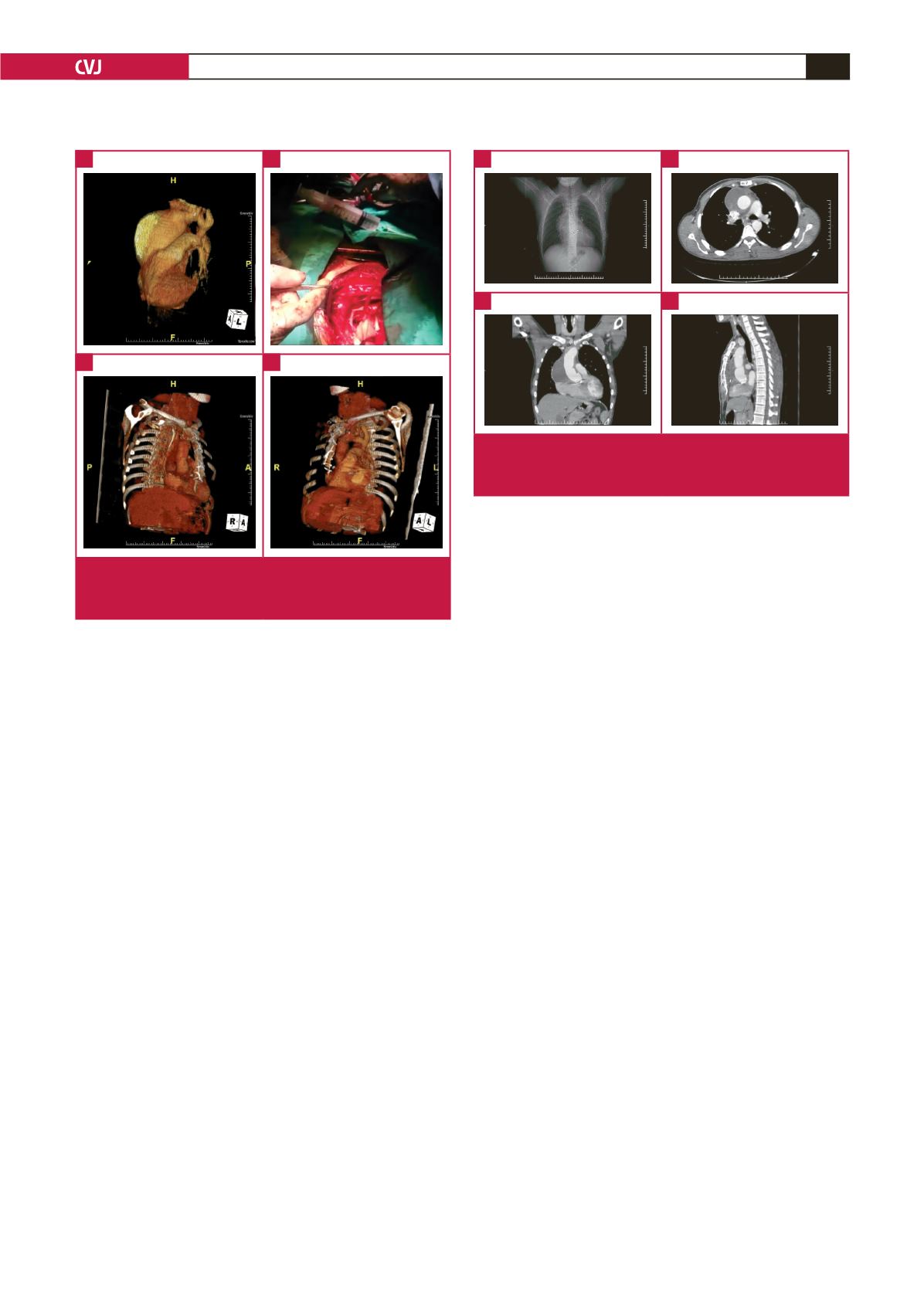
Fig. 2.
Pre-operative (A) and postoperative (C, D) three-
dimensional reconstructions from CT scans, and intra-
operative (B) view of the aortic aneurysm.
A
C
B
D
Fig. 3.
Postoperative radiography (A). Postoperative thoracic
CT scan: axial (B), coronal (C) and sagittal reconstruc-
tions – mediastinal window view (D).
A
C
B
D

















