
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 5, September/October 2017
AFRICA
287
suspected significance. Concomitant physical examinations,
including cardiac auscultation were not performed.
The completed studies were uploaded to a cloud-based web
server and stored using a picture archiving and communication
system (PACS) (Studycast; Core Sound Imaging, Inc, Raleigh,
North Carolina) and proprietary software (CoreConnect; Core
Sound Imaging, Inc). The transfer of the echocardiographic
images and data occurred via a secure broadband internet
connection, with CoreWeb validating the integrity and
confidentiality of the transmitted studies using standard secure
(SSL, TLS) encryption.
Post-screening echocardiographic analysis
Two certified professionals initially viewed each echocardiogram.
These included an echocardiographer and a paediatric
cardiologist with level III training in echocardiography (American
Society of Echocardiography), who separately interpreted and
reported on each archived echocardiographic examination using
a standardised format (SmartWorksheets
TM
, CoreWeb, North
Carolina). During this phase of analysis the readers were blinded
to individual demographic data.
The echocardiographic descriptions focused on findings
summarised in the WHF 2012 criteria for RHD and were
categorised as definite RHD, borderline RHD, or no RHD
(Table 1).
10
Physiological (non-pathological) tricuspid valve and
pulmonary valve regurgitation were noted, but not
comprehensively assessed unless there was significant co-existing
aortic and/or mitral valve pathology.
Subjects who were suspected of having echocardiographic
features of RHD or congenital heart disease were then referred
and examined by the Kigali-based paediatric cardiologists (JM,
ER) who are experienced in the diagnosis and management of
RHD, for subsequent management.
Statistical analyses
Data management and statistical analyses of all data were
performed (LM, VN, MS) at the Rwanda Biomedical Centre in
the Medical Research Centre in Kigali using STATA software
(Statacorp LP. College Station, Texas).
Descriptive statistics were performed; data were summarised
using frequency tables and graphs. Confidence interval of RHD
prevalence was computed at the 95% confidence level.
Results
Of the original 3 000 school children randomly selected,
2 693 (89.7%) underwent echocardiographic evaluation. However
on their scheduled day for screening, 307 were not present at
school or were not available. Of these 2 693 subjects, complete
demographic data from 2 501 subjects were available (92.8%; this
is 83.3% of the original 3 000 selected subjects) (Fig. 1).
The age distribution of the 2 501 subjects is shown in Fig.
2. The mean age of these 2 501 subjects who were completely
analysed was 11.2 years.
Of importance, 91% of the subjects undergoing diagnostic
echocardiography were students enrolled in the first six years of
primary school. Approximately 9% of those echocardiographic-
ally evaluated were somewhat older students (ages 16–20 years)
enrolled in the first three years of secondary school. Therefore,
the overall age distribution for the 2 501 subjects was weighted
towards younger school children.
Seventeen of the 2 501 children (0.68%) fulfilled the 2012 WHF
echocardiographic criteria for the diagnosis of RHD, in either the
definite or borderline category (Table 2, modified from reference 10).
Therefore, the RHD prevalence among this sample of 2 501 Rwandan
school children was 6.8/1 000 (95% CI: 4.2/1 000–10.9/1 000).
Characteristics of subjects meeting WHF criteria
for RHD
The age distribution of the 17 subjects with valvular RHD is
shown in Fig. 3. Of the 17 subjects who met the 2012 WHF
criteria, four (23.5%) were identified as definite RHD and 13
(76.5%) subjects were classified as borderline RHD (Fig. 4).
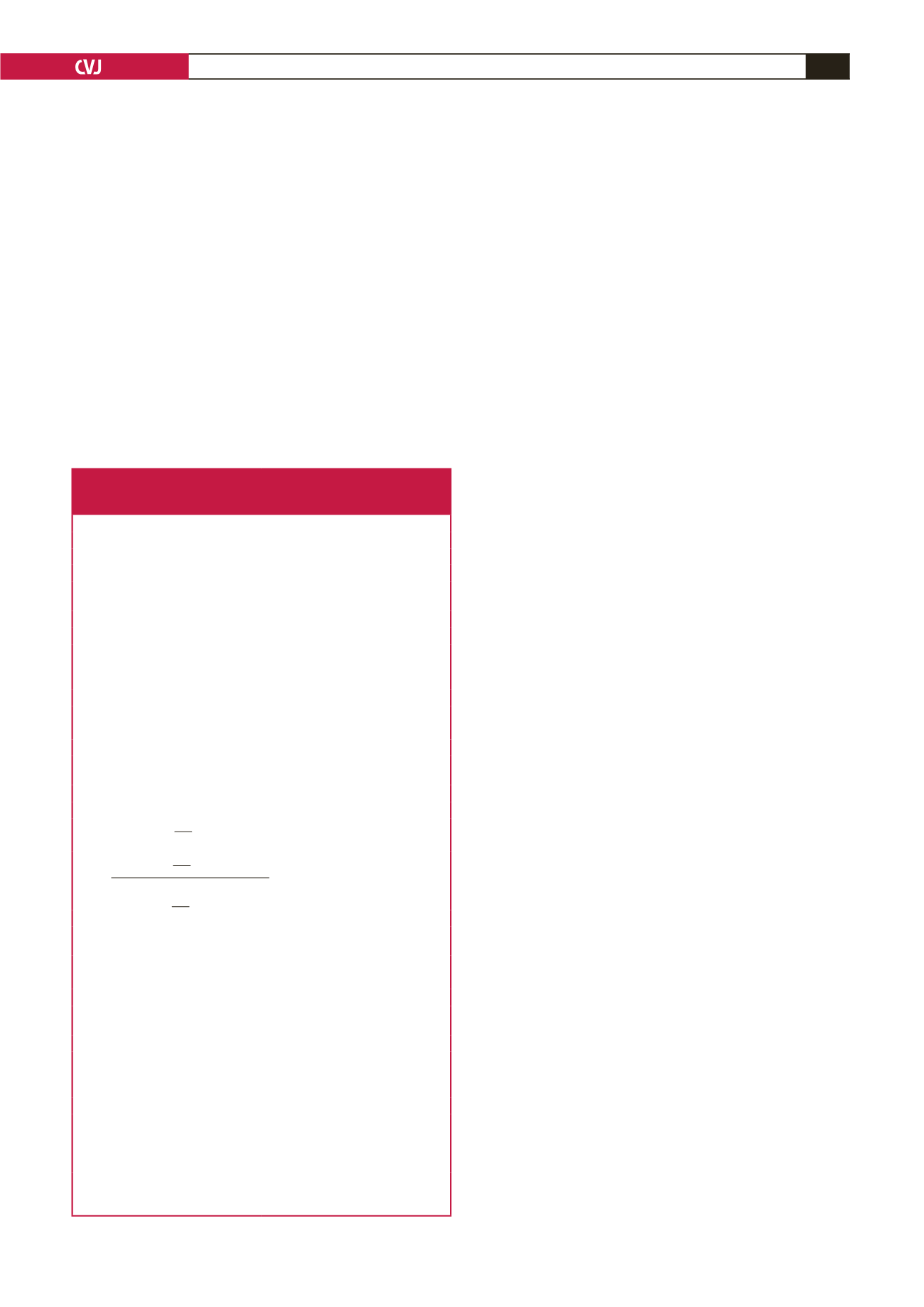
Table 1.World Heart Federation 2012 criteria for echocardiographic
diagnosis of rheumatic heart disease as applied to this study
(modified from reference 10).
Echo criteria for children
≤
20 years of age
Definite RHD (either A, B, C or D):
A) Pathological MR and at least two morphological features of RHD of the MV
B) MS mean gradient
≥
to 4 mmHg (NB – exclude congenital MV anomalies)
C) Pathological AR and at least two morphological features of RHD of the AV
(NB – exclude bicuspid aortic valve and dilated aortic root)
D) Borderline disease of both the aortic and mitral valves as defined below
Borderline RHD (either A, B or C):
A) At least two morphological features of RHD of the MV without pathologi-
cal MR or MS
B) Pathological MR
C) Pathological AR
Normal echocardiographic findings (all A, B and C);
A) MR that does not meet all four Doppler criteria (physiological MR)
B) AR that does not meet all four Doppler criteria (physiological AR)
C) An isolated morphological feature of RHD of the MV or the AV (e.g. valvar
thickening) without any associated pathological stenosis or regurgitation
Echo criteria for adults
>
20 years of age
Definite RHD (either A, B, C or D):
A) Pathological MR and at least two morphological features of RHD of the MV
B) MS mean gradient
≥
to 4 mmHg (NB – exclude congenital MV anomalies)
C) Pathological AR and at least two morphological features of RHD of the
AV in those under 35 years of age only. (Bicuspid AV and dilated aortic root
must first be excluded)
D) Pathological AR and at least two morphological features of RHD of the MV
Pathological regurgitation
Mitral regurgitation (all four Doppler
criteria must be met)
Aortic regurgitation (all four Doppler
criteria must be met)
1. Seen in two views
1. Seen in two views
2. In at least one view jet length
≥
2 cm 2. In at least one view jet length
≥
1 cm
3. Peak velocity
≥
3 m/s
3. Peak velocity
≥
3 m/s
4. Pansystolic jet for at least one
envelope
4. Pandiastolic jet for at least one
envelope
Morphological features of RHD
Mitral valve
Aortic valve
1. AMVL thickening
≥
3 mm
(age-specific)
1. Irregular or focal thickening
2. Chordal thickening
2. Coaptation defect
3. Restricted motion
3. Restricted motion
4. Excessive leaflet tip motion during
systole (hypermobile or flail leaflet)
resulting in abnormal coaptation
4. Prolapse
RHD, rheumatic heart disease; MR, mitral regurgitation; MV, mitral valve;
MS, mitral stenosis; AR, aortic regurgitation; AV, aortic valve; AMVL, anterior
mitral valve leaflet.

















