
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 6, November/December 2017
400
AFRICA
The articles comprised five RCTs from Brazil and Iran and
two non-RCTs from Argentina and Iran, as shown in Table 3.
11,14-19
Characteristics of the interventions across the seven studies are
detailed in Table 4. Six of the trials studied the impact of exercise
alone on maternal and birth outcomes, and one study investigated
using fortified food to enhance micronutrient nutritional status.
A study by Prevedel
et al
.
17
was one of two that used aquatic
physical activity as an intervention. The relative body fat
percentage of the experimental group remained at 29%, however,
the control group increased by 1.9%.
A study by Cavalcante
et al
.
18
also used an intervention of
aquatic exercise during pregnancy to determine its effectiveness
onmaternal outcomes. No differences were noted between control
and intervention groups for weight gain during pregnancy, body
fat percentage, fat-free mass or body mass index (BMI).
The effects of supervised aerobic exercise on the maternal
outcomes of overweight pregnant women were evaluated by
Santos
et al
.
14
Although oxygen consumption of the exercise
group at anaerobic threshold was higher post intervention,
neither groups showed any differences in weight change after the
intervention.
Two Iranian interventions
16,19
evaluated the effect of land-
based exercise on low-back pain during pregnancy. The typical
exercise programme for these studies included a combination of
midwife-supervised anaerobic and aerobic exercise performed
three days per week at a moderate intensity. In the study by
Garshabi
et al
.,
19
lordosis was reduced in the exercise group after
the intervention, but weight gain was similar between the study
groups. In addition, spinal flexibility was significantly lower in
the exercise group post intervention, and this was correlated
with BMI. Weight gain was lower in the control group, and body
weight of the neonate was higher than in the exercise group.
Although Sedaghati
et al
.
16
showed intensity of low-back pain
was higher in the control group, weight gain during pregnancy
was higher in the exercise group.
The intervention that aimed to determine the possibility
of improving maternal outcomes using fortified foods
11
found
that the prevalence of folic acid and serum retinol deficiency
decreased, while vitamin A deficiency remained the same post
intervention. No differences were noted for body composition,
and the proportions of overweight and obesity in the groups
were at a moderate level of 20 and 26.3%, respectively, post
intervention.
Discussion
Pregnancy appears to be a pivotal time for both maternal and
foetal health. Emerging research has highlighted the profound
effects of the
in utero
environment on the lifelong health of the
baby. More specifically, both underweight and overweight babies
are at risk of obesity later on in life.
20
The perinatal period has
been cited by Lawlor and Chaturvedi
21
as one of the three critical
periods in life for the prevention of obesity.
Maternal obesity is perhaps one of the major causes of intra-
uterine over-nutrition during pregnancy, and can lead to large-
for-gestational-age deliveries. In addition, excessive gestational
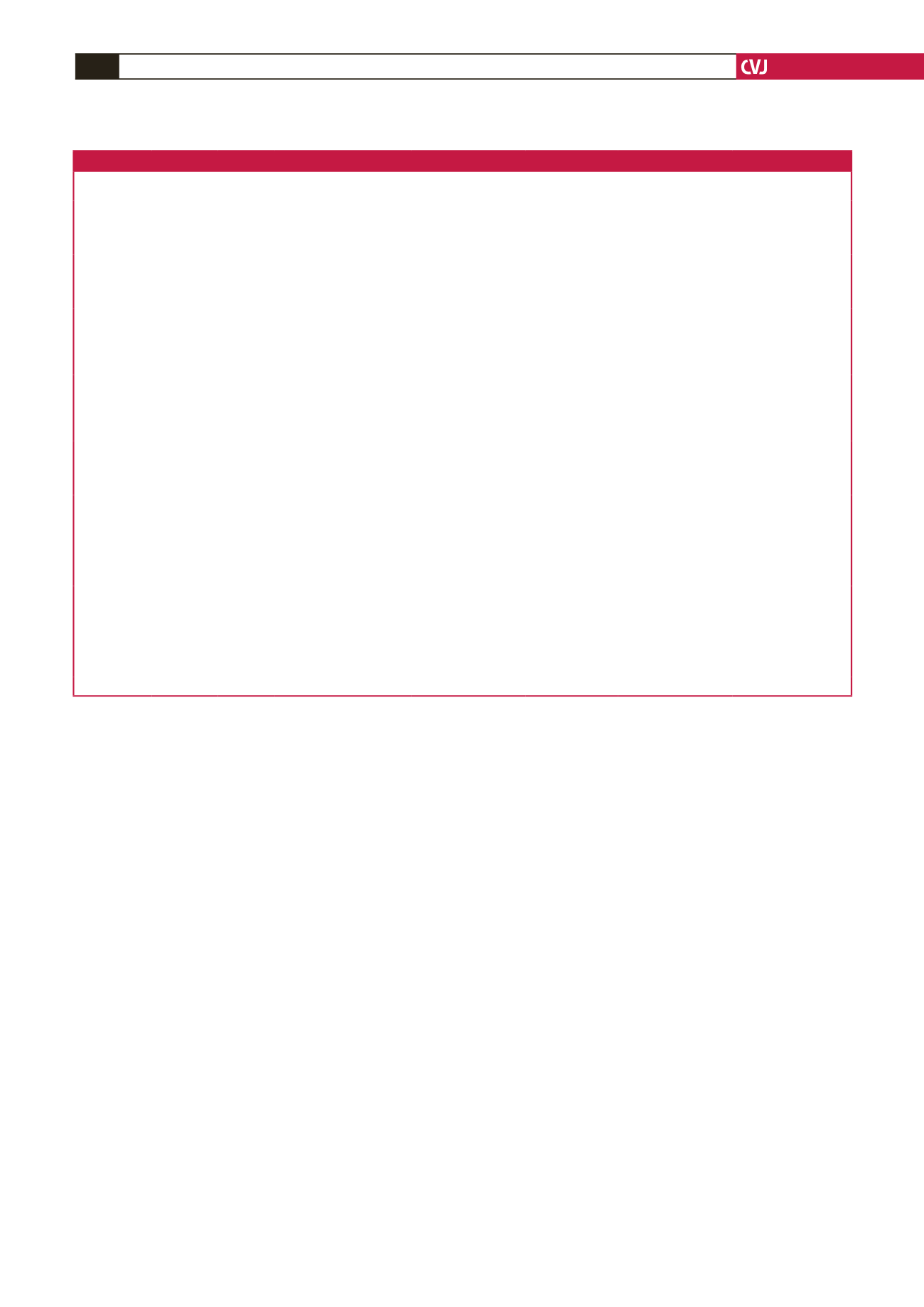
Table 3. Details and characteristics of the final studies included in the systematic review
Author
Type of
study
Country Region
Study setting
(urban/rural) Inclusion criteria
Sample size
Age (years)
Gestational age (weeks)
Santos
et al
.,
2005
14
RCT
Brazil
Porto
Alegre
Public health
clinic (not speci-
fied)
Healthy, non-smoking,
≥ 20 years, gestational
age < 20 weeks; BMI
26–31 kg/m
2
Control 35
Exercise 37
Control 28.6 ± 5.9
Exercise 26.0 ± 3.4
Control 18.4 ± 3.9
Exercise 17.5 ± 3.3
Garshasbi
et
al
., 2005
19
RCT
Iran
Tehran Hospital
Primi-gravid, 20–28
years old, 17–22 weeks’
gestation, housewives,
high-school graduated
Control 105
Exercise 107
Control 26.48 ± 4.43
Exercise 26.27 ± 4.87
Not specified
Malpeli
et al
.,
2013
11
Non-
randomised
Argentina Buenos
Aires
Urban
Sample from low-
income families, preg-
nant women, without
chronic or infectious
diseases
Control 164
Experimental 108
Control 25.8 ± 6.4
Intervention 26.3 ± 7.1
Control 23.6 ± 9.3
Intervention 24.3 ± 8.00
Sedaghati
et
al.
, 2007
16
Non-
randomised
Iran
Qom
province
Pre-natal clinics Exclusion: history of
orthopaedic diseases
or surgery, history of
exercise before preg-
nancy
Control 50
Experimental 40
Control 23.36 ± 4.237
Exercise 23.28 ± 2.522
Control 38.884 ± 1.232
Exercise 39.195 ± 0.921
Prevedel
et al.
,
2003
17
RCT
Brazil
Sao
Paulo
Pre-natal clinic
of the Faculty
of Medicine de
Botucatu (urban)
Primi-gravid or
adolescents, single-
ton pregnancies, no
co-morbidities
Intervention 22
Control 19
Mean: 20 years
16–20
Cavalcante
et
al
., 2009
18
RCT
Brazil
Sao
Paulo
Pre-natal out-
patient clinic of
the University of
Campinas and
the neighbouring
basic healthcare
centre
Low-risk, sedentary
pregnant women who
had not had more than
1 C-section and were
able to participate in
physical exercise
Intervention 34
Control 34
Not specified
16–20
Ghodsi &
Asltoghiri,
2012
15
RCT
Iran
Unspec-
ified
Pre-natal clinics
and hospitals
BMI 19.8–26 kg/m
2
;
lack of specific disease,
willingness to partici-
pate, correct address
for follow up; ability to
read and write; nulli-
and primi-gravid
Total sample 250;
unclear on
specific numbers
in each group
Control 25.86 ± 4.90
Training 25.43 ± 4.52
20–26
RCT = randomised, control trial; BMI = body mass index.

















