
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 6, November/December 2017
AFRICA
401
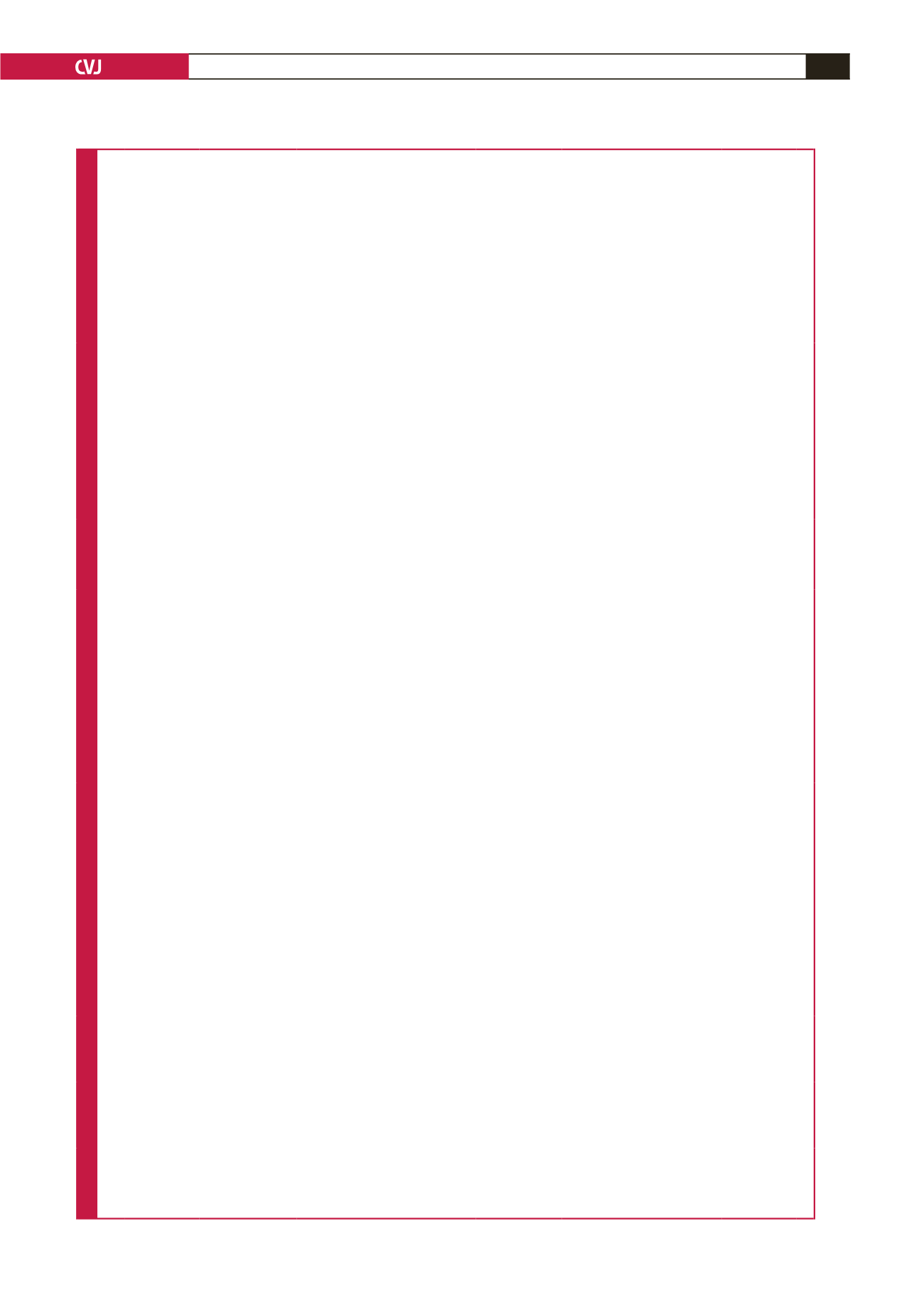
Table 4. Details and characteristics of the interventions in the studies
Author
Type of study
Intervention
(type) Intervention (details)
Intervention
(duration) Outcome measure
Pre-pregnancy
BMI/weight Weight/BMI
Conclusion
Santos
et al
.,
2005
14
RCT
Supervised
PA
60 min, 3 days/week, 5–10 warm up, 30 min heart
rate-monitored aerobic, 10–15 min upper- and lower-
limb exercise, 10 min relaxation. Aerobic: 50–60%
max HR ≤ 140 bpm
12 weeks Primary: O
2
consumption,
Secondary: respiratory
exchange ratio, CO
2
output,
HR, RHR, low birth weight,
prematurity, small for gesta-
tional age
Not specified Control: 27.5 ± 2.1, Exercise: 28.0 ±
2.1 (BMI); Baseline weight: control
71.2 ± 7.4, exercise 71.5 ± 7.9
Post-intervention weight: control 77.6
± 8.3, exercise 77.2 ± 9.1
Exercise group gained approximately 0.5
kg less over 12 weeks, but not statistically
significant (
p
= 0.62). Exercise sessions
during pregnancy were not associated with
low birth weight 3.363 ± 504 kg (exercise)
versus 3.368 ± 518 kg (control),
p
= 0.97.
Garshasbi
et
al
., 2005
19
RCT
Midwife-
supervised
exercise
3 days/week, 60 min, 5 min slow walking, 5 min
extension movements, 10 min general warm-up, 15
min anaerobic, 20 min specific exercise, 5 min return
to first position, HR ≤ 140 bpm
12 weeks Primary: intensity of low-
back pain, lordosis, flex-
ibility, maternal weight gain,
pregnancy length, neonatal
weight
Not specified Baseline weight: control 55.42 ± 12.90,
exercise 67.08 ± 12.8
BMI baseline: control 25.58 ± 5.12,
exercise 25.98 ± 4.82
Weight gain during pregnancy: control
13.8 ± 5.2, exercise 14.1 ± 3.8,
p
= 0.63
Weight of neonate: control 3 500 ± 431
g, exercise 3 426 ± 675 g
No significant difference between two
groups according to maternal weight gain
and neonatal birth weight. Exercise group
gained 0.3 kg more weight
Malpeli
et al
.,
2013
11
Non-
randomised
Nutritional
intervention
The nutritional intervention consisted of the month-
ly supply of a basic food basket containing 1 kg
fortified wheat flour (30 mg iron, 2 200 μg folic acid,
6.3 mg thiamine, 1.3 mg riboflavin, 13 mg niacin
per kg), 2 kg soy-enriched maize flour fortified with
micronutrients (1 500 μg RE vitamin A, 8 mg thia-
mine, 8 mg riboflavin, 100 mg niacin, 1,000 μg folic
acid, 40 mg iron, 30 mg zinc per kg), 1 kg sugar, and
1 kg rice. It also contained a nutritional supplement
(powder soup, 2 daily servings) equivalent to 250
Kcal daily, 270 μg retinol, 12 μg vitamin D, 20 mg
vitamin C, 0.7 mg vitamin B
1
, 0.7 mg vitamin B
2
, 0.9
mg vitamin B
6
, 0.9 μg vitamin B
12
, 6.8 mg niacin, 200
μg folic acid, 240 mg calcium, 35 mg magnesium, 6
mg iron, 4 mg zinc and 29 mg selenium.
1 year
Weight per trimester,
BMI per trimester, low
weight, normal weight,
overweight, obese, ferritin,
iron deficiency (prevalence),
folate, prevalence of folate
deficiency, zinc, prevalence
of zinc deficiency, retinol,
prevalence of vitamin A
deficiency
At baseline 27.5% were underweight;
25.4% normal weight; 22.4% over-
weight; 24.7% obese. There was a
significant decrease in folate deficiency
in the intervention group compared to
the control group. The risk of vitamin
A deficiency decreased significantly in
the intervention group.
No significant differences recorded between
intervention and control for anthropomet-
ric measurements. Energy and nutrient
intake was significantly increased in the
intervention group.
Sedaghati
et
al
., 2007
16
Non-
randomised
Midwife
supervised
exercise
15 min warm-up and cool-down, 30 min cycling
(55–65% MHR), 3 days/week, RPE 12–13,
Not
specified
Intensity of low-back pain,
maternal weight gain
Baseline BMI: control 24.30 ± 1.289,
exercise 24.10 ± 1.134
Baseline weight: control 61.04 ± 3.681
kg, exercise 60.78 ± 3.577 kg;
Weight gain: exercise group 13.55 ±
1.131 kg, control 15.10 ± 2.102 kg,
p
< 0.0001
Greater increase in weight gain was also
seen in the control group
Prevedel
et al.
,
2003
17
RCT
Aquatic
exercise
Hydrotherapy three times a week. Moderate inten-
sity for 1 hour at a time.
Until 36–40
weeks
Lean body weight (kg), total
fat (kg), relative fat (%), VO
2
max (ml/kg/min), systolic
volume (ml), cardiac output
(l/min), full-term/preterm
birth, baby’s weight (g)
Not specified Mean: 58 kg; height: 159–161 cm No difference in babies’ weight between the
two groups (3 175 g control group, 3 110
g intervention group). Significant findings
were: the mother’s relative fat percentage
increased in the control group but remained
the same in the intervention group. Systolic
volume and cardiac output increased in
the intervention group suggesting better
cardiometabolic maternal adaptation.
Cavalcante
et
al
., 2009
18
RCT
Aquatic
exercise
Water aerobics for 50 min three times a week.
Moderate intensity, 24.6 sessions per woman
Until 36
weeks’
gestation
Weight (kg), body fat (%),
fat-free mass (%), BMI,
% vaginal deliveries, %
preterm, neonatal weight
Intervention
63.8 ± 12.7,
control 60.8
± 10.2
Not specified
No significant difference seen between
the two groups for any of the outcome
measures.
Ghodsi &
Asltoghiri,
2012
15
RCT
Mixed
aerobic and
flexibility
exercise
Mixed exercise regime including stretching and
flexibility and aerobic exercises (swimming, cycling,
walking) three times a week
20–26th
week until
delivery
Neonatal weight; 1st and 5th
APGAR scale
Not specified 19.8–26 kg/m
2
Mean BMI for training group was 23.4
± 1.9 and 23.3 ± 2.1 for the control
group
No significant difference in neonatal weight
between the training and control group (3
204 g vs 3 216 g, respectively). No signifi-
cant differences in APGAR scale between
the two groups. No reporting on maternal
weight as an outcome
PA = physical activity; min = minutes; RCT = randomised controlled trial; BMI= body mass index; HT = heart rate; RHR = relative heart rate.

















