
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
275
Out of 59 children with positive HHE results, 34 were
available for a SE study while 15 were unable to attend due to
social reasons and 10 were travelling. Of the 34 children who
underwent SE, 29 were found to have RHD (85.2%); 22 had
definite and seven borderline disease. The ratio of definite-to-
borderline RHD by SE was 3.1:1, with females representing 72%
of the definite cases. The echo prevalence was 19/1 000 children.
The bias-adjusted kappa test showed good agreement between
the two echo readers of 92.9% (= 2, Agreement 1 = 2 × 0.9643
– 1).
All the cases with definite and borderline RHD were asked
to come for a follow-up study by SE after six months. Definite
RHD cases were started on benzathine penicillin prophylaxis.
Table 2 and Figs 1 and 2 summarise these findings.
Table 3 details the echo findings of 29 cases found positive
using SE. MR was present in all the cases detected by SE and
in 58/59 of those by HHE (Fig. 3). AR was present in seven
cases using HHE (11.8%) and in four with SE. Of those with
AR detected by HHE, only four came for SE. Two children had
aortic valve morphological abnormalities detected by HHE but
did not come for SE. These included irregular thickening in one,
and in another case it was associated with leaflet prolapse and
asymmetry (Fig. 4). No cases of mitral or aortic stenosis were
identified.
The agreement between HHE and SE on the assessment
of mitral valve morphological criteria as well as the diagnosis
of RHD were calculated. Bias-adjusted kappa showed a fair
agreement of anterior mitral valve leaflet thickness > 3 mm,
chordal thickening and excessive leaflet tip motion in systole (28,
28 and 32%, respectively) and good agreement (66%) with the
diagnosis of definite versus borderline RHD.
Discussion
This is the first study that has measured the echo-diagnosed
prevalence of RHD in Sudan. This was coupled with the
initiation of a control programme based on training of health
personnel, and raising public awareness in South Darfur.
Compared with the 1992 clinical prevalence of 11 per 1 000,
3
RHD prevalence in Khartoum has dropped significantly, which
could be attributed to the relative improvement of health services
and living conditions in urban areas. On the other hand, this
study unmasked a huge burden of asymptomatic patients living
in a poor rural community. In sharp contrast to Khartoum, the
prevalence in South Darfur camps was over 60 times higher. This
prevalence may have been underestimated due to the smaller
sample size and the high number of children who could not
attend the SE study in Niyala.
The Khartoum study was conducted by paediatric cardiology
fellows who were experienced in echo and were using three echo
views as per the modified WHF protocol, therefore the accuracy
of the echo studies was expected to be high. Moreover, the inter-
observer agreement was 92%, indicating the reliability of echo
interpretation. This disparity in prevalence could be attributed
to many factors, including the availability of more health centres
within Khartoum compared to the Darfur area, and a relatively
better socio-economic status and more secure living conditions
in the Mayo area, which is only 9 km from the Khartoum centre.
The ratio of definite-to-borderline RHD cases of 3:1 further
supports the notion that the disease is well established in Darfur
Total number
screened = 1515
Total number
analysed = 1498
Positive by HHE = 59
Definite = 44
Borderline = 15
Those who had
SE = 34
Positive cases by SE = 29
Definite = 22
Borderline = 7
Fig. 2.
Total subjects screened in Darfur and their results.
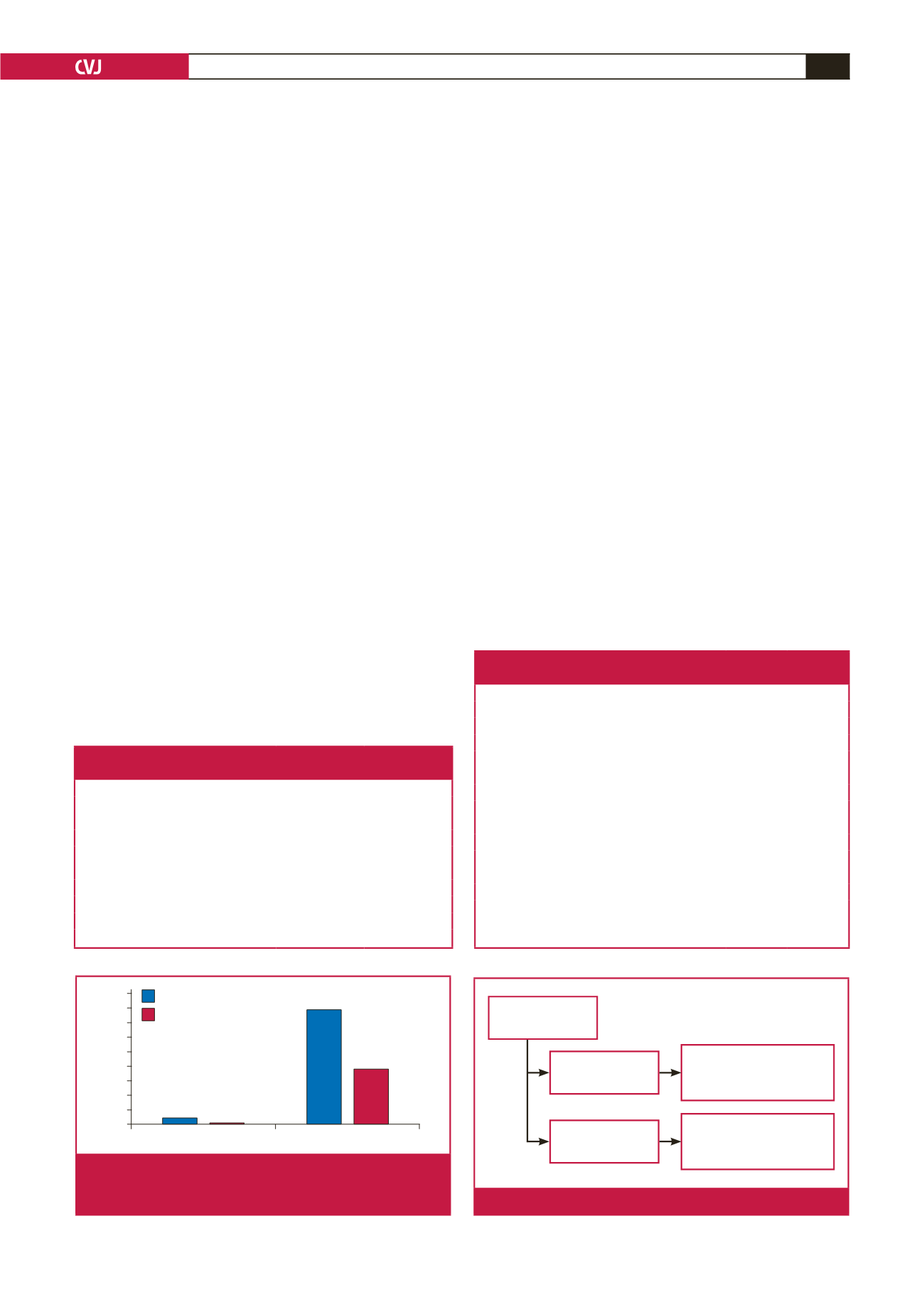
Khartoum
Niyala-Darfur
45
40
35
30
25
20
15
10
5
0
HHE
SE
Fig. 1.
Prevalence of RHD in Khartoum and Niyala, Darfur
(per 1 000 population) by hand-held echo (HHE) and
standard echo (SE).
Table 2. Summary of the clinical and echo findings
of children in Khartoum and Niyala, Darfur
Characteristics
Khartoum Niyala, Darfur
Number of school children
3 000
1 515
Number of echo studies analysed
3 000
1 498
Mean age in years (± SD)
10.5 (0.4)
10.8 (0.2)
Female gender (%)
50
51
Echo findings
Positive by HHE
7
59
Positive by SE
1
29/34
Definite-to-borderline ratio using HHE
0.16/1
2.9/1
RHD prevalence using echo
0.3/1 000
19/1 000
Table 3. Features of patients who were found
to have RHD by standard echo (total = 29)
Patient characteristics
No (%)
Type of RHD
Definite
22 (76)
Borderline
7 (24)
Female:male ratio
3:1
Echo features
Definite Borderline
Pathological MR
22 (100)
7 (100)
AML thickening
18 (81)
4 (57)
Chordal thickening
22 (100)
4 (57)
Restricted leaflet motion
1 (0.04)
0
Excessive anterior leaflet tip motion
13 (59)
0
Pathological AR
4 (18)
0
Morphological aortic valve criteria
0
0
Borderline disease in both mitral and aortic valves
3 (14)
0
MR: mitral regurgitation, AML: anterior mitral valve leaflet, AR: aortic regur-
gitation.

















