
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
279
We obtained the data for these patients from the records of
our catheterisation laboratory. Patients who had had acute
myocardial infarction and totally occluded coronary lesions were
excluded from the study.
A total of 147 patients with 155 lesions between them
were identified and retrospectively enrolled in the study in a
consecutive manner. These patients’ records were evaluated for
visual estimation of their lesion severity by two other operators
who were blinded to the previous primary operator’s visual
estimation. We also categorised the lesions as percentages
according to their severity:
<
50, 50–69, 70–89 and 90–99%.
Three visual estimations (qualitative evaluation) were therefore
obtained for each lesion.
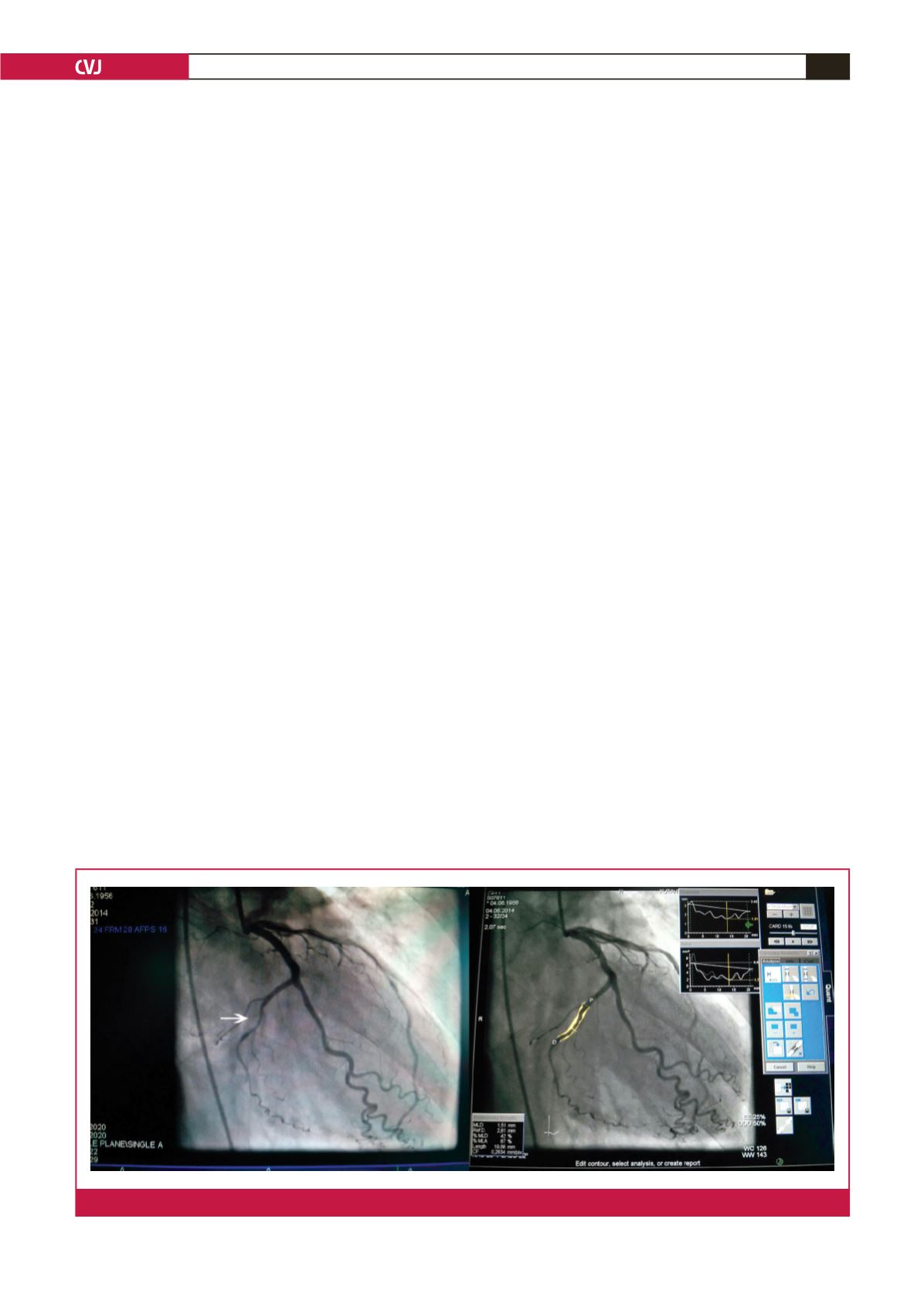
For QCA analysis, first, the lesion was evaluated in multiple
views for quality of the images, excessive foreshortening, side-
branch overlap and severity of stenosis. The frame demonstrating
the most severe narrowing with the best image quality and least
foreshortening was selected in end-diastole and then calibration
was done using the tip of the catheter. Disease-free segments of
proximal and distal coronary segments were used as reference
segments.
Thereafter, the software automatically detected the contour
after manually tracing a central line through the lesion. The
proximal and distal coronary segments should be relatively free
of disease and were referred to as the reference diameter. Vessel
contour was automatically detected by the software and edge
detection was corrected if necessary. In cases of multi-lesion
intervention, each lesion was evaluated separately (Fig. 1).
Complete QCA analysis of the lesions of each patient was
performed by another operator who was blinded to the visual
assessment of the lesions. Reference diameter (the diameter of
the disease-free segments of the proximal and distal vessels),
minimal lumen diameter, percentage of stenosis, percentage
area of stenosis and lesion length from the proximal lesion-
free segment to the distal lesion-free segment in diameter
were calculated using a computerised QCA software program
(Axiom Artis Zee, Siemens, Germany). One QCA (quantitative
evaluation) measurement was thus obtained for each lesion.
Statistical analysis
Continuous variables are expressed as mean
±
SD and categorical
variables as numbers and percentages. All data were evaluated by
IBM SPSS (Statistical Package for Social Sciences, version 22).
Kappa analysis was used for evaluation for concordance of
visual assessments between operators. The difference between
visual assessment and QCA was determined using the paired
Student’s
t
-test. Concordance between visual assessment and
QCA was tested with kappa analysis. The difference between
percentage diameter of stenosis and percentage area of stenosis
was assessed with the paired Student’s
t
-test.
Results
The study population was composed of 147 patients who
underwent PCI for 155 lesions between them. Table 1 shows the
characteristics of the patients and the 155 lesions. Mean age of
the patients was 64.7 years (range 28–95). There were 107 men
(72.8%) and 42 women (27.2%).
The mean percentage of stenosis of the 155 lesions determined
visually by the primary operator was 84% (range 55–99). The
most commonly reported category for percentage of stenosis by
the primary operator was 70–90%. The most treated vessel was
the left anterior descending artery (LAD) (68, 46.4%), followed
by the right coronary artery (RCA) (42, 27.1%), the circumflex
artery (Cx) (39, 25.2%) and the intermediate artery (two, 1.3%).
In total, 159 stents were implanted. Five patients underwent
balloon dilatation only, 92 underwent bare-metal stent
implantation, whereas 56 had drug-eluting stent implantation.
Both bare-metal and drug-eluting stents were implanted in two
patients. Mean stent length was 19.1
±
6.6 mm (range 8–54).
Mean stent diameter was 3.13
±
0.49 mm (range 2.0–4.75).
Mean percentages of stenosis determined by the primary,
second and third operator by visual estimation were 84.0, 80.4
and 80.4%, respectively (Table 2). Concordance between the
operators was evaluated with kappa (
κ
) analysis. There was a
moderate degree of concordance in the categories 70–89% (
κ
:
0.406) and 90–99% (
κ
: 0.5813), while in the categories
<
50 and
Fig. 1.
Quantitative coronary analysis of a lesion in the left circumflex coronary artery.

















