
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
308
AFRICA
useful in outcome measures.
Inazumi
et al
. found that cystatin C levels were more accurate
for mortality prediction than eGFR in patients with ADHF.
23
They showed that even without a decrease in eGFR, increases
in cystatin C level were associated lower long-term, event-free
survival (180 days). Also, Rafouli-Stergiou
et al
. reported
that in-hospital rise in cystatin C and NT-proBNP levels was
useful in predicting 60-day cardiac death and rehospitalisation.
24
Similarly, we found that, rather than estimated GFR calculations,
in-hospital mortality rate was related to higher cystatin C and
NT-proBNP levels. However, during long-term follow up, only
sodium level was an independent predictor of death, which
affirms that hyponatraemia is a surrogate marker for mortality.
25
Interestingly, we found that younger patients were more
prone to suffer a cardiac death than older subjects. The possible
reason for this finding may be that our hospital is a tertiary
referral centre for heart transplant candidates, and younger
patients with a worse clinical condition are mostly referred to
our centre for advanced therapies. When we looked at similar
studies evaluating mortality differences in ADHF patients, they
principally included older subjects (60 years or more),
11,23,24
with
an absence of younger patients, which might have limited data on
differences in mortality rates in such patients.
Compared to the above studies, including younger patients
may add further information about the association between
cystatin C levels and mortality rates in such populations.
Furthermore, among patients who died during their hospital
stay, the rate of prior cerebrovascular accident was significantly
higher than among survivors. The presence of cerebrovascular
accident is a risk factor for HF,
26
but the co-existence of these
conditions may be related to increased mortality rate.
In the ASCEND trial, 180-day follow up of patients with
ADHF showed that baseline cystatin C level was a strong
predictor of adverse events.
27
However, increase in cystatin
C levels did not predict adverse outcomes. In contrast to the
ASCEND trial, we did not observe differences in mortality rate
with regard to baseline cystatin C levels during the 36-month
follow-up time. Despite the fact that the sample size of our study
was small, our results provide complementary data for long-term
follow up of subjects with ADHF and raised cystatin C levels.
Although our study had a prospective design and followed
patients for a considerable period, the number of recruitedpatients
was relatively small, which probably lowered the statistical power
of the study. Also, the recruited patients represent a relatively
young population compared to previous studies. Because our
centre is a tertiary referral hospital, the patient characteristics
may not represent the whole HF population. Finally, we
did not analyse GFR, cystatin C and plasma NT-proBNP
levels according to heart failure aetiology, and only admission
levels were evaluated rather than follow-up values. The cost-
effectiveness of serial measurements of cystatin C levels in the
prognostication of HF patients should be confirmed in large
prospective studies.
Conclusion
In subjects with ADHF, evaluation of admission cystatin C levels
may provide a reliable prediction of death compared to eGFR or
NT-proBNP levels. Higher cystatin C levels provided important
prognostic data about unfavourable in-hospital outcomes. For
the post-discharge follow-up period, sodium level was the marker
that had prognostic significance.
The preliminary results of this study (in-hospital mortality) were accepted as
an oral presentation at the American College of Cardiology congress in 2013
(http://dx.doi.org/10.1016/j.cardfail.2013.06.088). The three-year follow-up
results were accepted as an abstract presentation at the European Society of
Cardiology Heart Failure congress (21–24 May 2016) in Florence, Italy.
References
1.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney
disease and the risks of death, cardiovascular events, and hospitaliza-
tion.
N Engl J Med
2004;
351
: 1296–1305.
2.
Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to
serum creatinine as a marker of kidney function: a meta-analysis.
Am J
Kidney Dis
2002;
40
: 221–226.
3.
Taub PR, Borden KC, Fard A, Maisel A. Role of biomarkers in the
diagnosis and prognosis of acute kidney injury inpatients with cardiore-
nal syndrome.
Expert Rev CardiovascTher
2012;
10
: 657–667.
4.
Lassus J, Harjola VP. Cystatin C: a step forward in assessing kidney
function and cardiovascular risk.
Heart Fail Rev
2012;
17
: 251–261.
5.
GarcíaAcuña JM, González-Babarro E, Grigorian Shamagian L, Peña-
Gil C, Vidal Pérez R, López-Lago AM,
et al
. Cystatin C provides more
information than other renal function parameters for stratifying risk
in patients with acute coronary syndrome.
Rev Esp Cardiol
2009;
62
:
510–519.
6.
Naruse H, Ishii J, Kawai T, Hattori K, Ishikawa M, Okumura M,
et al
.
Cystatin C in acute heart failure without advanced renal impairment.
Am J Med
2009;
122
: 566–573.
7.
Dupont M, Wu Y, Hazen SL, Tang WH. Cystatin C identifies patients
with stable chronic heart failure at increased risk for adverse cardiovas-
cular events.
Circ Heart Fail
2012;
5
: 602–609.
8.
Bruneau BG, Piazza LA, de Bold AJ. BNP gene expression is specifically
modulated by stretch and ET-1 in a new model of isolated rat atria.
Am
J Physiol
1997;
273
: H2678–2686.
9.
Gustafsson F, Steensgaard-Hansen F, Badskjaer J, Poulsen AH, Corell
P, Hildebrandt P. Diagnostic and prognostic performance of N-terminal
ProBNP in primary care patients with suspected heart failure.
J Card
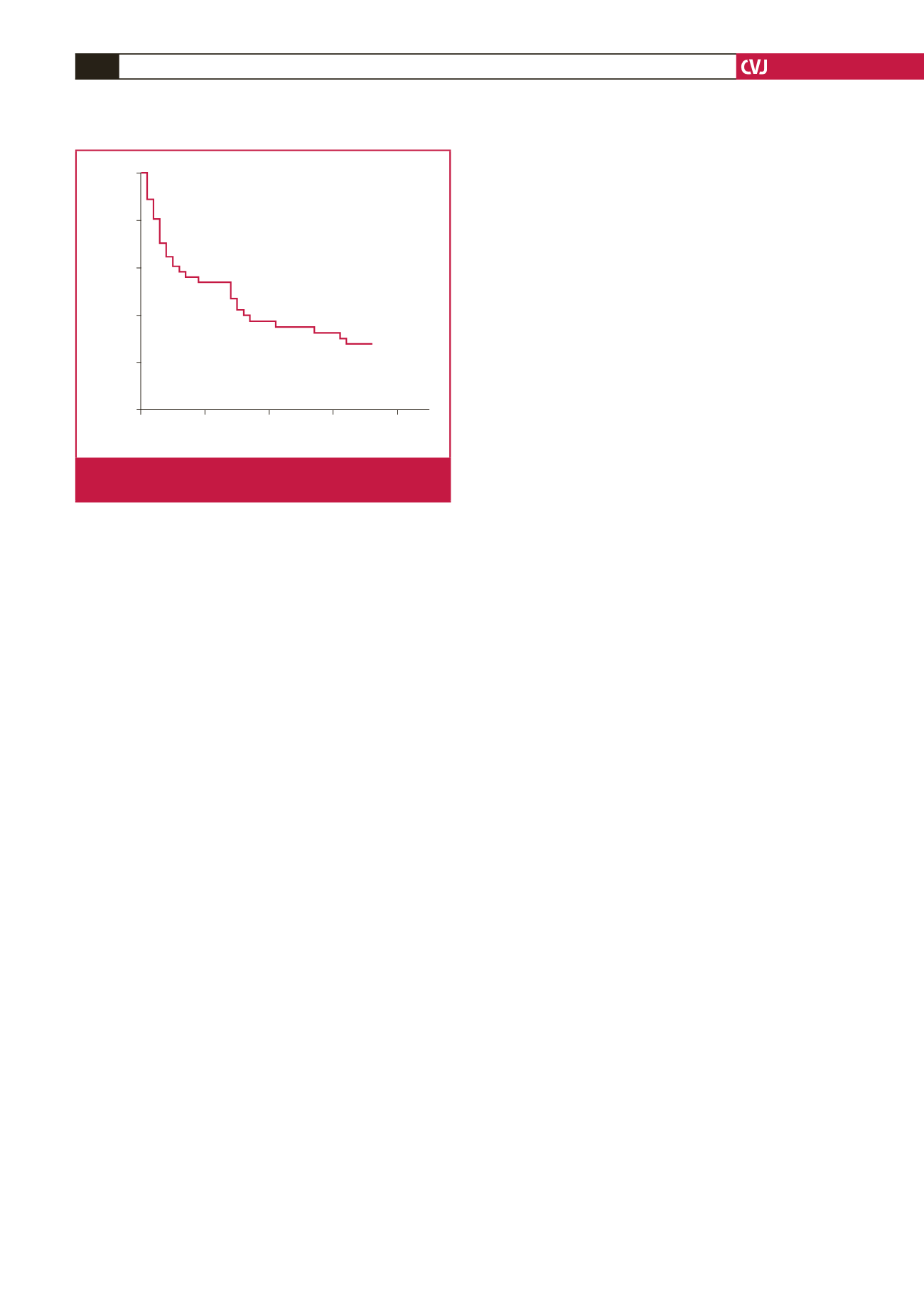
Months
0
10
20
30
40
Cumulative survival
1.0
0.8
0.6
0.4
0.2
0
Fig. 1.
Plot of the survival curve for patients with acutely
decompensated heart failure.

















