
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 5, September/October 2018
AFRICA
313
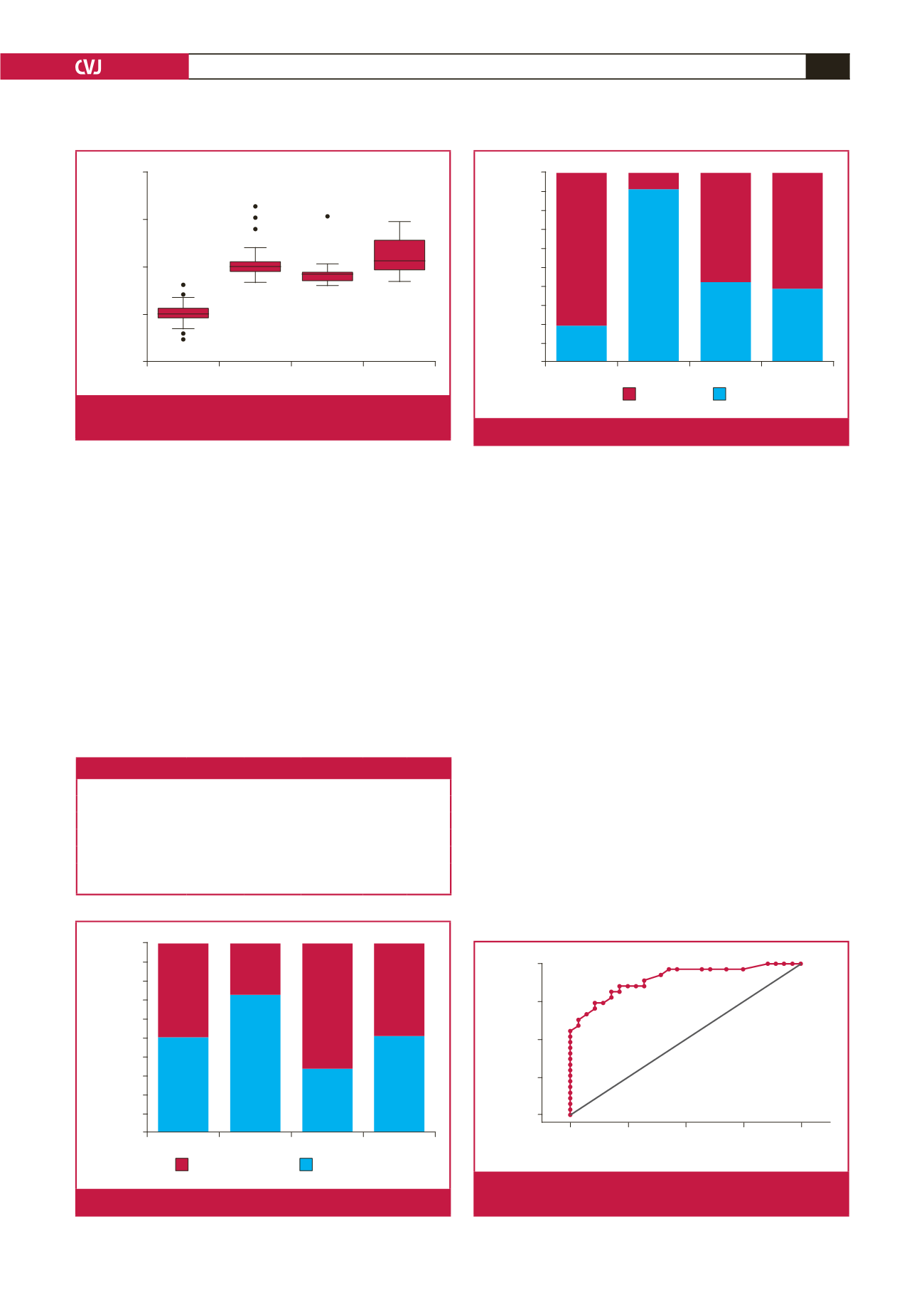
PE-only and PE–IUGR groups, respectively (Fig. 4). This
difference was statistically significant (
p
<
0.001).
The utility of MPI in predicting adverse outcomes was
assessed. We found that the MPI
z
-scores served as a good
marker of an adverse obstetric event later in pregnancy, as
evidenced by the total area under the curve (AUC) of 0.90. The
ROC curve is presented in Fig. 5. A cut-off value of 4.5 on the
MPI
z
-score conferred a sensitivity of 89% and specificity of
68% (Table 3).
We also assessed the accuracy of a CPR value less than
the fifth percentile in predicting adverse outcomes. Fig. 4
demonstrates CPR categorisation between the groups. Table 4
demonstrates the utility of CPR in predicting adverse outcomes.
Of the 54 cases with CPR values, 33 (61%) had values less than
the fifth percentile (p5). The sensitivity of CPR
<
p5 in predicting
adverse events was 66% and the specificity was estimated at 42%
(Table 4).
Logistic regression was performed to evaluate predictors of
adverse events after adjusting for all other foetal parameters.
In univariate logistic regression, MPI
z
-score, AFI, EFW, UA
Doppler, CPR category, DV Doppler and MCA Doppler were
assessed separately as potential predictors of adverse outcomes.
The only significant predictor of adverse outcome was the MPI
z
-score. Treating this as a continuous variable, the odds ratio was
7.8 (95% CI: 2.3–26.1), which can be interpreted as follows: for
a one unit higher Mod-MPI
z
-score, there is an approximately
eight-times higher risk of an adverse outcome.
Discussion
We have previously shown that mainly in severe IUGR, that
is, compensated and critical-status IUGR and in severe early-
onset pre-eclampsia, an elevated MPI was a good predictor of
adverse neonatal outcome, and cut-off MPIs were suggested.
5,6
This study now focused on whether an elevated MPI in milder
forms of placental-mediated disease was a predictor of adverse
obstetric outcome later on in the pregnancy. This study has
shown that a cut-off value of 4.5 on the MPI
z
-score is a strong
indicator of adverse obstetric outcome later in pregnancy, with
Control
IUGR PE-only PE–IUGR
MPI
z
-score
15
10
5
0
–5
Fig. 2.
Mpi
z
-score versus controls, IUGR, PE-only and PE
+
IUGR groups.
Table 2. CPR versus adverse events
IUGR PE-only PE–IUGR Total
p
-value
Adverse events,
n
(%)
16 (50)
3 (27)
8 (67)
27 (49)
0.197
CPR
<
0.001
>
p5
6 (19)
10 (91)
5 (42)
21 (38)
<
p5
26 (81)
1 (9)
7 (58)
34 (62)
CPR
=
cerebro-placental ratio, IUGR
=
intra-uterine growth restriction, PE
=
pre-eclampsia.
IUGR PE-only PE–IUGR Total
Adverse event rate (%)
100
90
80
70
60
50
40
30
20
10
0
16
Adverse event
No adverse event
3
8
27
16
8
4
28
Fig. 3.
Adverse-event rate between groups.
IUGR PE-only PE–IUGR Total
CPR categorisation (%)
100
90
80
70
60
50
40
30
20
10
0
26
< p5
> p5
1
7
34
6
10
5
21
Fig. 4.
CPR categorisation between groups.
0.00
0.25
0.50
0.75
1.00
Sensitivity
1.00
0.75
0.50
0.25
0.00
1 – Specificity
Area under ROC curve = 0.8981
Fig. 5.
ROC curve depicting diagnostic accuracy of MPI
z
-scores.

















