
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 6, November/December 2018
AFRICA
369
and log cotinine). Changes (
Δ
) were calculated using the formula:
Δ =
follow up – baseline. Coping measures included DefS, social
support, avoidance, cognitive/emotion, spiritual-, collectivistic-
and ritual-centred scores.
Independent
t
-tests and chi-squared (
χ
²) tests compared coping
and BP differences in means and proportions between black
and white respondents at baseline, respectively. The
t-
test for
dependent sampling compared ethnic differences over time.
McNemar’s case–control tests were used to demonstrate changes
in depression, hypertension, and usage of anti-hypertensive
medication over three years, and odds ratios (OR) and 95%
confidence intervals (CI) were determined. Logistic regression
analyses were computed to determine (1) changes in coping
scores over three years predicting chronic depression (PHQ-9
≥
10); and (2) changes in depressive symptoms predicting 24-hour
hypertension, independent of
a priori
covariates. A sensitivity
analysis was done by repeating logistic regression analyses to
adjust for HIV-positive status and use of hypertension medication.
The statistical significance level was set at
p
≤
0.05 (two-tailed).
Effect sizes when comparing means or proportions are reported
as
d
-values with 0.2
=
small effect, 0.5
=
medium effect and 0.8
=
large effect. When reporting OR as an effect size, the following
guideline values can be used: 1.5
=
small effect, 2.5
=
medium
effect and 4.25
=
large effect.
24
Results
Interaction terms showed ethnic differences for
Δ
24-hour DBP
[
F
(1.355)
=
5.04;
p
=
0.025] and
Δ
social support [
F
(1.353)
=
38.6;
p
≤
0.001]. These findings were used to stratify participants
into ethnic groups.
Cross-sectional investigation
Table 1 compares baseline characteristics of the two ethnic
groups. Cardiovascular risk was higher in blacks compared
to whites (
p
≤
0.001), with mean values exceeding known
cut-off points with medium to large effects (
d
-values
>
0.5; BP:
24-hour SBP
≥
130 mmHg and/or 24-hour DBP
≥
80 mmHg).
Blacks similarly showed statistically significantly higher risk for
psychosocial stress, i.e. longer exposure to an urban-dwelling
lifestyle, more alcohol consumption (
γ
-GT), and less physical
activity compared to whites (
p
≤
0.001), with a medium to
large effect. Blacks had increased 24-hour heart rate, 24-hour
hypertension, and used more anti-hypertensive medication than
whites (
p
≤
0.001; medium effect). Coping scores indicated that
whites used more avoidance coping coupled with less social-
support-seeking coping strategies (
p
≤
0.001; medium and
large effects). Blacks also reported the use of more cognitive/
emotional, spiritual-centred, collectivistic- and ritual-centred
coping than whites (
p
≤
0.001; medium to large effects).
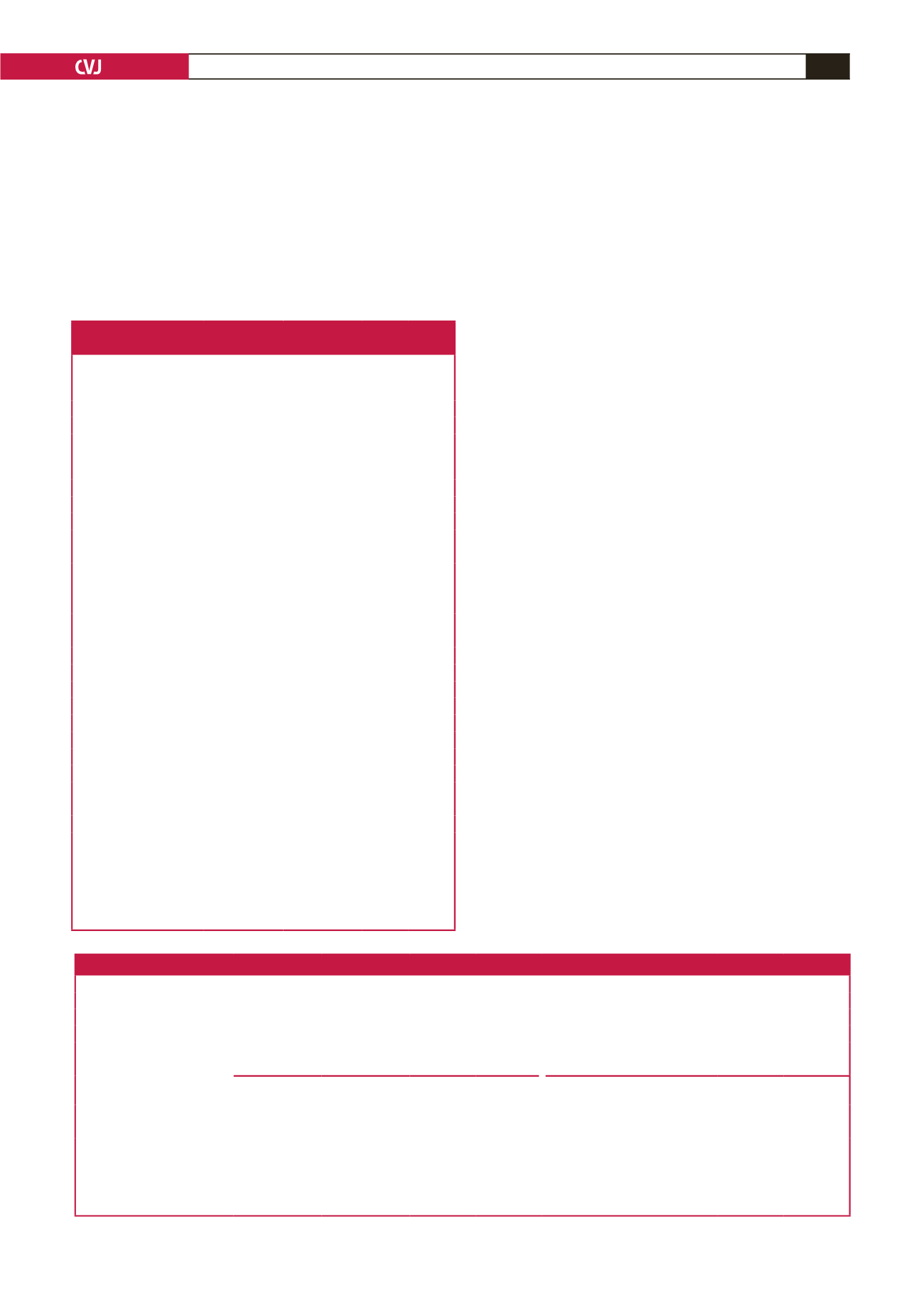
Table 1. Clinical characteristics of a bi-ethnic
South African teacher’s cohort at baseline
Characteristics
Blacks
(
n
=
173)
Whites
(
n
=
186)
p
-values
d
-values
Age, years
44.5 ± 7.8
46.6 ± 9.9
0.03 –0.21
Women,
n
(%)
84 (48.6)
95 (51.1)
0.63 –0.07
Urban living, years
32.0 ± 16.0
20.7 ± 12.4
<
0.001 0.71
Cotinine, ng/ml
26.8 ± 59.5
24.1 ± 81.0
0.72 0.03
Gamma-glutamyl
transferase, U/l
68.0 ± 83.8
28.0 ±35.3
<
0.001 0.48
Physical activity, kcal/24 h 2689.8 ± 812.7 3048.4 ± 826.7
<
0.001 –0.43
Waist circumference, cm 93.7 ± 14.9
93.6 ± 16.2
0.98 0.01
Depressive symptoms
9.4 ± 5.4
5.6 ± 4.6
<
0.001 0.70
Coping scores (CSI)
Defensive
28.2 ± 4.2
29.0 ± 3.8
0.052 –0.19
Social support
25.6 ± 7.8
18.7 ± 4.9
<
0.001 0.88
Avoidance
21.1 ± 3.8
23.8 ± 5.2
<
0.001 –0.52
Culture–specific coping scores (ACSI)
Cognitive emotion
15.9 ± 6.7
10.0 ± 5.8
<
0.001 0.88
Collectivistic-centred
12.6 ± 5.4
8.6 ± 4.2
<
0.001 0.74
Ritual-centred
2.4 ± 2.4
0.4 ± 0.9
<
0.001 0.83
Spiritual-centred
13.4 ± 6.1
11.3 ± 5.3
<
0.001 0.34
Cardiovascular risk
HbA
1c
, %
6.1 ± 1.3
5.5 ± 0.4
<
0.001 0.46
24-h SBP, mmHg
133 ± 16
125 ± 12
<
0.001 0.50
24-h DBP, mmHg
84 ± 11
77 ± 8
<
0.001 0.64
24-h PP, mmHg
49 ± 9
47 ± 7
0.03 0.22
24-h heart rate, bpm
80 ± 10
74 ± 10
<
0.001 0.60
HIV,
n
(%)
15 (8.7)
0 (0)
<
0.001 0.44
CVD history,
n
(%)
16 (9.3)
21 (11.3)
0.525 –0.07
24h hypertension,
n
(%)
a
114 (66)
81 (44)
<
0.001 0.43
Anti-hypertensive usage,
n
(%)
62 (35.8)
26 (14.0)
<
0.001 0.51
SBP
=
systolic blood pressure; DBP
=
diastolic blood pressure; PP
=
pulse pres-
sure; HIV
=
human immune-deficiency virus infection; CVD, cardiovascular
disease history.
a
Hypertensive status classified as 24-h SBP
≥
130 mmHg and/or 24-h DBP
≥
80
mmHg. Values are mean (± SD).
Table 2. Comparing qualitative and quantitative lifestyle changes over a three-year period in blacks and whites
Blacks (
n
=
173)
Whites (
n
=
186)
p
-values
d
-values
Qualitative attempts at lifestyle changes after 3 years
Smoking,
n
(%)
17 (10)
9 (5)
0.069
0.17
Alcohol consumption,
n
(%)
24 (14)
6 (3)
≤
0.001
0.31
Diet,
n
(%)
40 (23)
36 (23)
0.383
0.09
Blacks (
n
=
173)
Whites (
n
=
186)
Baseline/
follow up
Difference
(95% CI)
p
-values
d
-values
Baseline/
follow up
Difference
(95% CI)
p
-values
d
-values
Quantitative lifestyle changes at 3-year follow up
Cotinine, ng/ml
27.0/33.1
6.0 (–3.3, 15.4)
0.203
0.27
24.1/21.6
–2.4 (–7.1, 2.2)
0.307
–0.03
γ
GT, U/l
67.6/60.9
–6.7 (–15.7, 2.2)
0.138
–0.08
28.0/27.1
–0.9 (–5.0, 3.1)
0.647
–0.03
WC, cm
93.7/98.1
4.3 (3.2, 5.6)
≤
0.001
0.29
93.6/96.3
2.6 (1.6, 3.6)
≤
0.001
0.16
γ
GT, gamma-glutamyl transferase; WC, waist circumference.
Values presented as arithmetic mean at baseline/follow up as well as the difference over three years (95% CI).
p
-values were obtained from dependent
t
-tests;
d
-value effects: 0.2
=
small; 0.5
=
medium; 0.9
=
large.

















