
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 3, May/June 2020
AFRICA
159
Perspective
The acute coronary syndrome revisited: effects and
therapeutic modulation of excess metabolic fuel supply
M Faadiel Essop, Lionel H Opie*
Our proposal is that that metabolic perturbations occurring during
and after the onset of the acute coronary syndrome (ACS) require
careful management from the moment patients with this diagnosis
are admitted to the intensive care unit (ICU). We advocate that
insulin treatment should be initiated when blood glucose levels
rise to above 11 mM (or 200 mg/dl), thereby providing additional
therapeutic benefits. The reasons are as follows.
Metabolic substrate alterations in ACS
Physiologically the heart relies on a mixture of exogenously
supplied substrates (predominantly long-chain fatty acids) for
ATP production and for muscle contraction. The main source for
the heart’s high demand for ATP is oxidative phosphorylation of
ADP in the respiratory chain. Metabolism of energy-providing
substrates produces the reducing equivalents for the proton
gradient across the inner mitochondrial membrane. The collapse
of this proton gradient transfers energy to ATP.
Neurohumoral stress alters substrate supply
and utilisation in the heart
Increased sympathetic nervous system (SNS) activation during
the ACS triggers the stimulation of sympathetic fibres within
the myocardium, leading to greater norepinephrine/epinephrine
discharge. This ‘fight or flight’ response has profound metabolic
consequences. The adrenal medulla simultaneously releases
epinephrine that suppresses pancreatic
β
-cell insulin secretion
and in parallel elevates hepatic gluconeogenesis and myocardial
glycogenolysis. In addition, higher SNS activation enhances
cortisol production (adrenal cortex) that results in downstream
stimulation of hepatic gluconeogenesis. Therefore high
circulating catecholamine levels associated with the ACS elicit a
robust increase in both blood free fatty acids (FFA) and glucose
concentrations and a concomitant decrease in insulin levels that
may persist for several hours, resulting in detrimental effects on
the ischaemic heart.
Damaging effects of high FFA levels
The concept that high circulating plasma FFA damage the
ischaemic myocardium is well established. For example,
isolated hearts perfused with high FFA levels display abnormal
contractility and heart rhythm,
1
and also increased myocardial
oxygen uptake. This effect can be explained by FFA-mediated
uncoupling of mitochondrial respiration, leading to oxygen
‘wastage’ and attenuated ATP production.
2-4
Excess FFA
availability and myocardial uptake also influences glucose–
fatty acid interactions, whereby elevated
β
-oxidation of fatty
acids lowers mitochondrial glucose utilisation (at the pyruvate
dehydrogenase step), and, to a lesser extent, attenuates glucose
uptake. Such FFA-induced metabolic abnormalities can be
lessened by the promotion of glucose metabolism when both
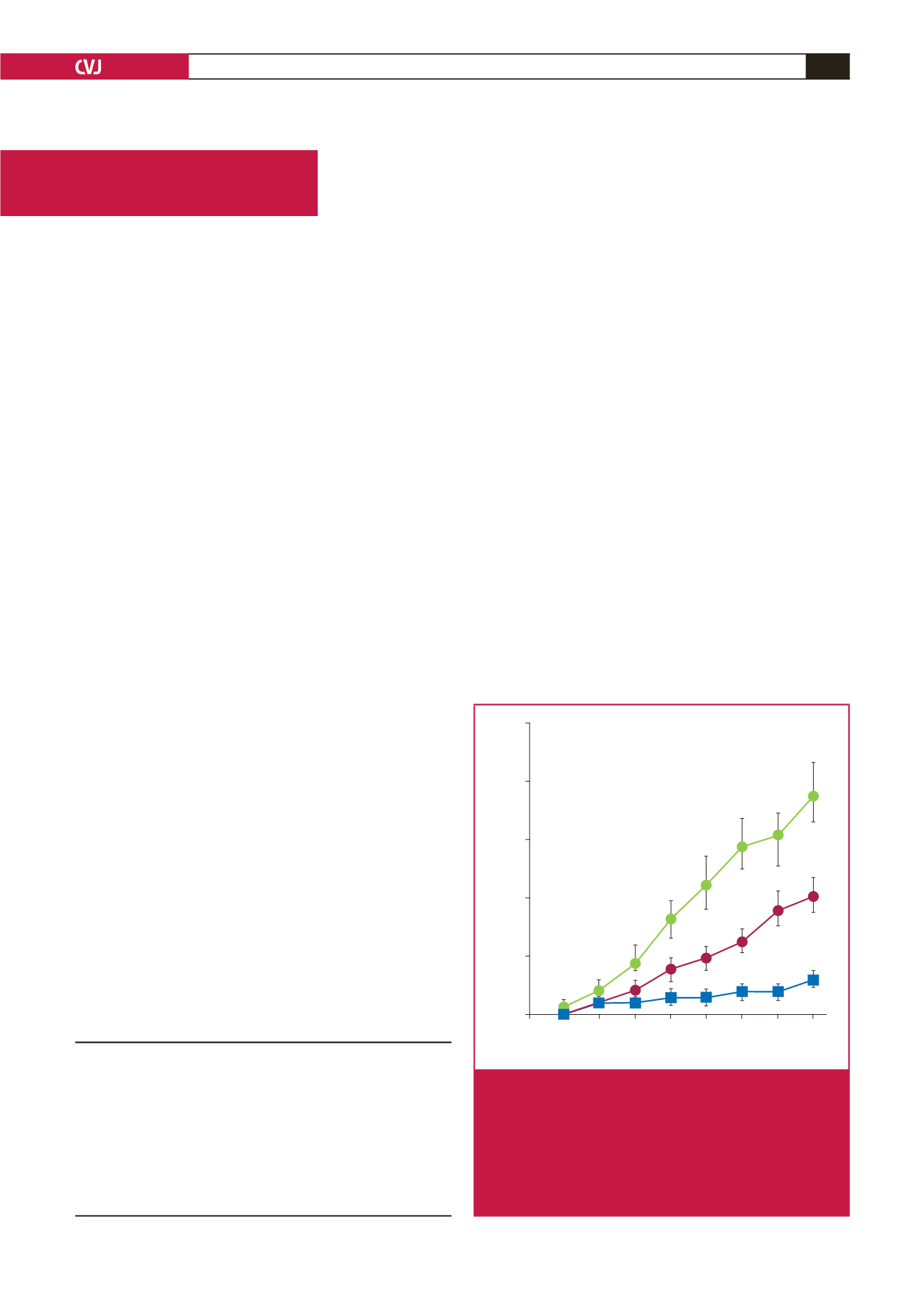
glucose and insulin are added to the perfusate (see Fig. 1).
5
These
observations are particularly relevant to the heart in diabetes,
which is already exposed to high systemic FFA and glucose
levels.
Centre for Cardio-Metabolic Research in Africa,
Department of Physiological Sciences, Stellenbosch
University, Stellenbosch, South Africa
M Faadiel Essop, PhD,
mfessop@sun.ac.zaHatter Institute for Cardiovascular Research in Africa,
Department of Medicine, University of Cape Town and
Groote Schuur Hospital, Cape Town, South Africa
Lionel H Opie, MD, PhD
*Deceased 20 February 2020
50
40
30
20
10
0
–15 0 15 30 45 60 75 90 105
Minutes after ligation
LDH release U/g wet wt/h
Fig. 1.
In experimental regional ischaemia, the addition of
high free fatty acids (FFA) (as 5:1 molar ratio for
palmitate:albumin) increased enzymatic release as
lactate dehydrogenase (LDH) release (top line) versus
lower FFA (palmitate:albumin ratio of 1:1) (middle
line).
5
This release indicated the extent of tissue
damage, which was reduced by added glucose and/or
insulin (
p
< 0.004) (bottom line).



















