
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
AFRICA
239
involvement of the heart in HIV-infected patients.
9
However, it
appears that HAART converted symptomatic cardiac disease
to mild or asymptomatic disease in one study,
14
significantly
improving patient survival and quality of life. Our study was not
powered to draw any conclusions as to the effect of HAART
on incidence of cardiac involvement, since we did not compare
patients on ART with those who were not.
We also performed TDI studies on both the LV and RV
(Table 2). TDI has been shown to unmask subtle abnormalities
that were not detected by conventional echocardiography.
32,33
Some important abnormalities were observed in our patients. A
significant proportion of patients who had normal findings on
conventional echocardiography had shown abnormal MPI, LV
diastolic dysfunction and RV systolic and diastolic dysfunction
on TDI. MPI, which involves load, heart rate and ventricular
geometry, and is an independent measure of systolic and
diastolic ventricular function, was also abnormal for both
ventricles in our group of patients compared to critical cut-off
points and
Z
-scores set by multiple investigators in the past,
23,34-37
indicating the presence of subclinical LV and RV dysfunction.
MPI includes both diastolic and systolic time intervals and is a
sensitive marker of ventricular systolic and diastolic function,
even when it is unrecognisable by conventional echocardiography.
Our study attempted to show an association between
patient clinical factors such as age, gender, BMI, World Health
Organisation clinical stage, previous treatment for opportunistic
infections, CD4 count, age at initiation of HAART, duration
of HAART and having a specific type of cardiac involvement
such as increased LV mass index, LV diastolic dysfunction, or
RV systolic/diastolic dysfunction. We did not find a statistically
significant association. We then considered an association
between such patient factors and having any of the cardiac
abnormalities combined (Table 3). Although there was a
tendency towards an association, none of these reached a
statistically significant level. Previous work by different authors
has also reported inconsistent associations between such factors
and cardiac involvement in children living with HIV.
4,13,16,38
Our study has important limitations. First, interpretation
of TDI findings was based on previously set reference values
and
Z
-scores. However, this has its own drawbacks and the
more appropriate way would have been to take a control
group of healthy children and adolescents matched for age
and gender. Second, there were other important and relevant
echocardiographic indices that we did not measure due to
logistical issues.
Conclusion
Our sample of children and adolescents living with HIV
had subclinical cardiac abnormalities detected on conventional
echocardiography as well as TDI. While few patients had
abnormalities detectable on conventional echocardiography,
such as reduced LV ejection fraction, pulmonary hypertension
and pericarditis, a larger proportion of patients had subtle
abnormalities, such as increased MMI, LV diastolic dysfunction,
RV dysfunction and abnormal MPI. However, to make better
sense of the TDI indices, it would probably have been better
to compare with a group of healthy children, drawn from a
similar socio-demographic background. Our study did not
show a strong association between specific patient factors and
echocardiographic abnormalities in this sample of patients.
We thank the staff of the Paediatric Infectious Disease Clinic for facilitating
the data-collection process. We are grateful to all patients who consented to
participate in this study. Our thanks go to Dr Dejuma Yadeta, who reviewed
our manuscript and gave us constructive comments. Last but not least, we
thank the Department of Paediatrics and Child Health for approving and
allowing the study to be conducted.
References
1.
UNAIDS: Global HIV and AIDS statistics fact sheet. World AIDS
DAY December 1 2018.
http://www.unaids.org. Accessed December
2018.
2.
Agwu AL, Fairlie L. Antiretroviral treatment, management challenges
and outcomes in perinatally HIV-infected adolescents.
J Int AIDS Soc
2013;
16
: 1–13.
3.
Chelo D, Wawo E, Siaha V,
et al
. Cardiac anomalies in a group of
HIV-infected children in a pediatric hospital: an echocardiographic
study in Yaounde, Cameroon.
Cardiovasc Diagn Ther
2015;
5
: 444–453.
4.
Miller RF, Kaski JP, Hakim J,
et al.
Cardiac disease in adolescents with
delayed diagnosis of vertically acquired hiv infection.
Clin Infect Dis
2013;
56
: 576–582.
5.
Lipshultz SE, Easley KA, Orav EJ,
et al.
Left ventricular structure
and function in children infected with human immunodeficiency virus:
The Prospective P2C2 HIV Multicenter Study.
Circulation
1998;
97
:
1246–1256.
6.
Starc TJ, Lipshultz SE, Easley KA, et al. Incidence of cardiac abnor-
malities in children with human immunodeficiency virus infection: the
prospective P2C2 HIV study.
J Pediatr
2002;
141
: 327–334.
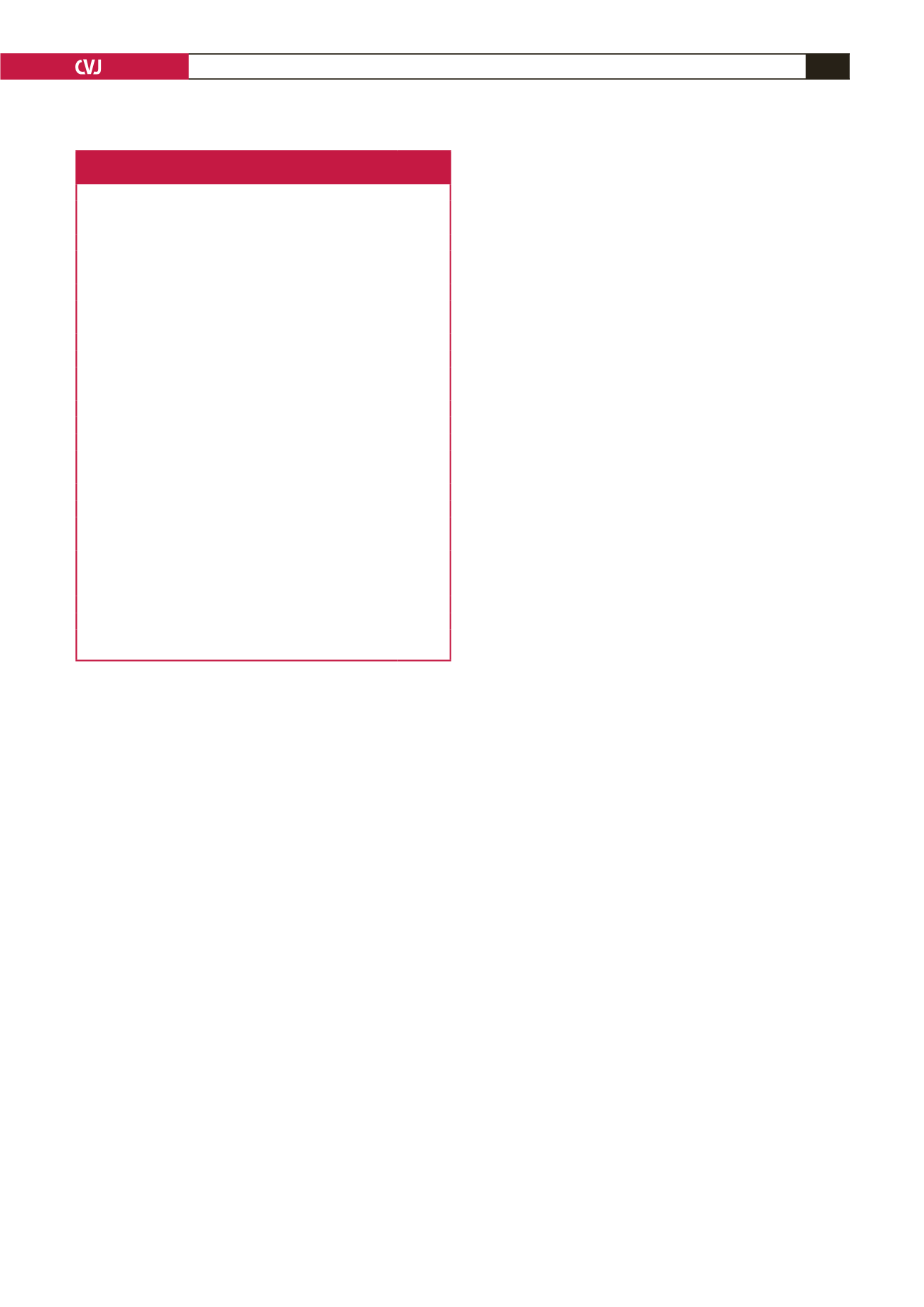
Table 3. Factors associated with cardiac abnormalities in
151 HIV-infected children and adolescents on HAART
Variables tested for association
Abnormal echo findings
p
-value
Age at time of study (years)
≤ 12
22/57
0.728
> 12
33/94
Gender
Female
28/83
0.498
Male
27/68
Body mass index
Z
-scores
<
–2
11/26
0.511
≥ –2
44/124
Initial WHO clinical stage
I and II
15/55
0.082
III and IV
40/96
Lowest CD4 count
<
200
39/97
0.220
≥ 200
16/54
Age at initiation of HAART (years)
<
9
11/80
0.490
10–13
14/59
14–19
2/12
Duration of HAART (months)
<
24
11/29
0.894
≥ 24
45/121
Previous treatment for opportunistic
infections (per WHO definition)
Yes
33/78
0.131
No
22/73
WHO, World Health Organisation; HAART, highly active antiretroviral treat-
ment; LV, left ventricular.



















