
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
64
AFRICA
followed by class III (37.1%) and class IV (8.8%). Atrial fibrillation
was documented in 13.8% of patients. Only three children (0.9%)
satisfied the modified Jones criteria for ARF at presentation, with
a further 31 subjects (9.7%) satisfying the criteria for active carditis
during follow up, yielding a total of 34 subjects with active carditis
(10.6%). MR was classified as moderate in 76 (23.8%) and severe in
244
(76.2%) patients, based on clinical assessment and confirmed at
echocardiography.
Co-morbidity was encountered in 44 patients (13.75%). The
main co-morbidity was HIV infection, which was found in 33
patients (10.3%), all of whom were on antiretroviral therapy. The
exclusion of 277 patients with uncontrolled hypertension (SBP >
140 mmHg, DBP > 90 mmHg while on treatment, on two separate
visits) resulted in only four patients with hypertension being enrolled
into the study.
Overall, heart failure occurred in 117 (36.6%) patients during
their illness; of these 23 (19.7%) had heart failure on their initial
admission. At the first visit, infective endocarditis was diagnosed
clinically in three patients in whom echocardiography showed valve
prolapse associated with vegetations. Of these, one patient was
subsequently diagnosed as ARF with carditis. In the second patient,
the anti-streptolysin O titre (ASOT) was elevated and at surgery,
chordal elongation was identified with no evidence of endocarditis.
In the last patient, chordal rupture was present at surgery but there
was no evidence of endocarditis, and subsequent blood cultures
failed to culture an organism.Echocardiographic findings revealed
a mean LVEF of 60.6 ± 8.3% with 52.5% of patients having
LVEF < 60%. The mean EDD and ESD were 60.0 ± 8.1 and 38.8
± 7.5 mm, respectively. Pulmonary hypertension was present in
the majority (
n
= 256, 80%) of subjects. Of these, 140 (54.6%)
patients had severe pulmonary hypertension; 55 (39.3%) were in
the paediatric age group, 37 (26.4%) were adults over 25 years
of age and 48 (34.3%) were in the middle age group. Associated
tricuspid regurgitation (TR) with pulmonary hypertension was
present in 172 (53.75%) patients and the severity of TR was
classified as mild in 74 (43.0%), moderate in 44 (25.6%) and
severe in 54 (31.4%) subjects. It was considered secondary to
pulmonary hypertension in most of the patients, except for nine
(5.23%) who had organic rheumatic tricuspid valve disease.
MR was classified as moderate in 76 (23.8%) and severe in
244 (76.2%) patients, based on clinical assessment and confirmed
at echocardiography. We categorised the echocardiographic
findings based on the Carpentier classification of leaflet motion
as normal (type 1), excessive (type 2) or restricted motion (type
3A), and recorded the anatomical descriptions of the entire valve
apparatus relating to the annulus, leaflet, commissures, chords
and papillary muscles. In keeping with the rheumatic aetiology,
increased leaflet thickness was reported in all but one patient
(99.7%), but commissural fusion was documented in only four
(1.2%) patients.
The majority of our patients had Carpentier type 2 leaflet
dysfunction with leaflet prolapse present in 196 (61.3%) and
chordal rupture identified in 118 (37%) subjects. The posterior
mitral leaflet was described as rigid, or having restricted mobility
(Carpentier IIIa) in 64 (20%) patients in our study, with
thickening of the subvalvular apparatus in 48 (15%) patients.
Calcification was found in 27 (8.4%) patients and reported to be
severe in one.
A posteriorly directed eccentric jet was present in 97% of cases.
The anatomical and functional pattern of regurgitation was quite
different from MR due to the rare congenital atrioventricular
canal defects associated with mitral valve anomalies such as
clefts and bridging leaflets. The commonest pattern of RHD that
emerged was that of an eccentric regurgitant directed posteriorly
with excessive leaflet motion (Carpentier type 2), due mainly
to anterior mitral valve leaflet prolapse as a result of chordal
elongation or chordal rupture and associated with increased
leaflet thickness. Together with annular dilatation, this was the
predominant mechanism of MR in the younger subjects and
suggestive of ongoing carditis.
Although annular dilatation was not documented by the
echocardiographer, the ESD > 60 mm and EF < 60% in half the
subjects suggested that the majority of subjects also had mitral
annular dilatation. This was supported by the large size of the
prostheses inserted by the surgeon in the cases that proceeded
to surgery.
Patients were divided into two age groups based on age
(seven to 25 years, and over 25 years) (Table 2) for comparison.
Although there was no significant difference in the proportion of
individuals having moderate or severe MR, or in the degree of
Table 1. Demographic data
Characteristics
7–12 years
(
n
= 116)
13–25 years
(
n
= 108)
> 25 years
(
n
= 96)
Overall
(
n
= 320)
Age (mean ± SD) years 9.7 ± 1.7 17.4 ± 4.0 42.7 ± 12.9 22.2 ± 15.8
Gender (%)
Male
39.7
34.3
20.8
32.2
Female
60.3
65.7
79.2
67.8
Ethnicity (%)
Asian
0
0.9
12.5
4.1
Black
100.0
97.2
81.3
94.1
Coloured
0
0
1.0
0.3
Unknown
0
0.9
1.0
0.6
White
0
0
3.1
0.9
*Other: concomitant congenital heart disease, renal failure, pericardial
diseases and non-valvular cardiomyopathy.
MR: mirtral regurgitation, MS: mirtral stenosis.
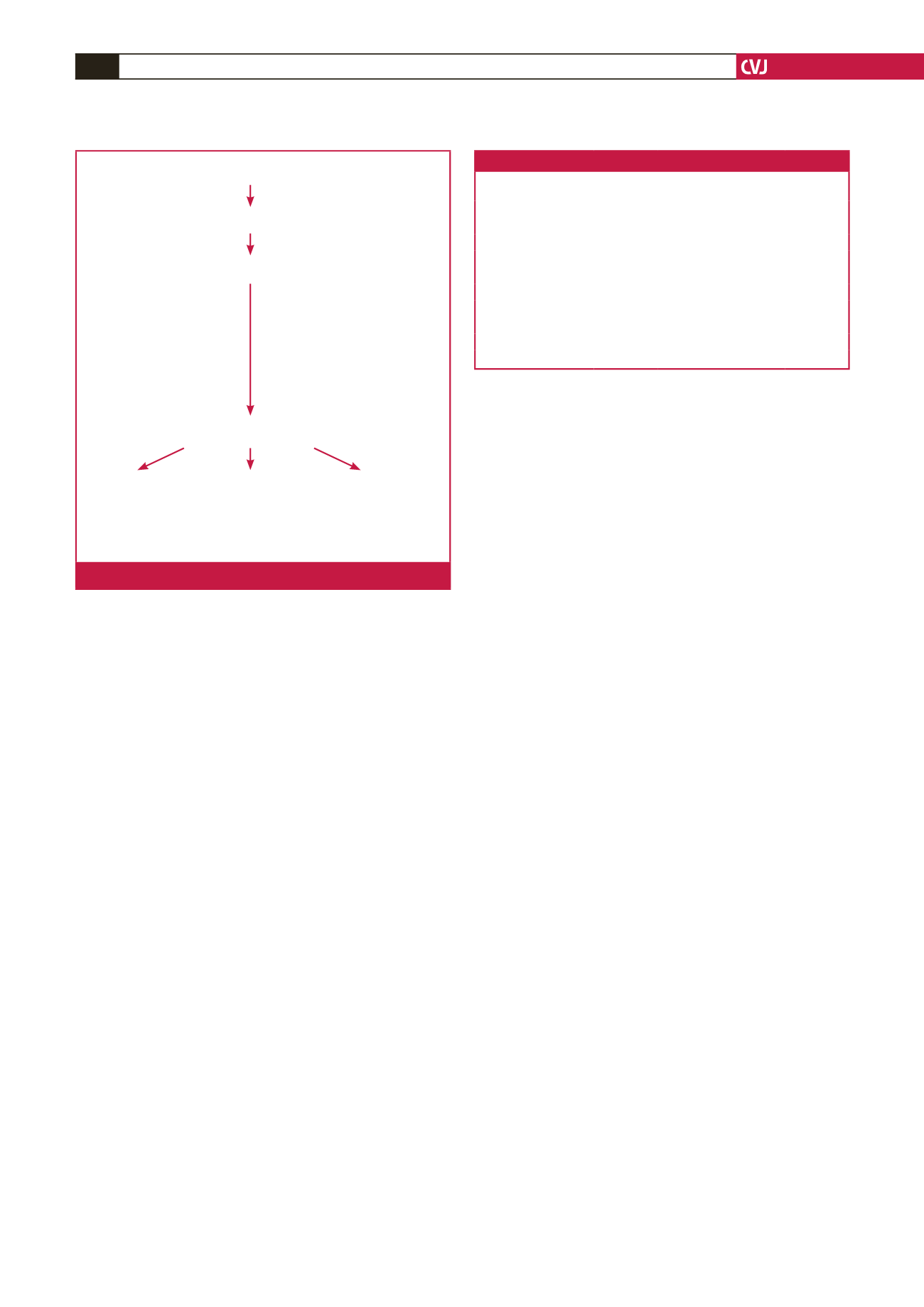
n
= 2 986 rheumatic MR
– 613 dominant MS
2 373 patients
– 1 106 presented to
non-cardiac disciplines
1 267 patients admitted for cardiology evaluation
– 201 mitral stenosis
(valve area < 2.0 cm
2
)
– 277 uncontrolled hypertension
– 157 aortic valve disease
– 91 pregnancy
– 75 non-rheumatic MR
(misclassified)
– 7 mild MR
– 2 severe anaemia
(not due to infective endocarditis)
– 137 other*
320 study patients with isolated MR
7–12 years:
n
= 116 13–25 years:
n
= 108 > 25 years:
n
= 96
Fig. 1.
Selection of the study sample.



















