
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
AFRICA
59
Editorial
Atrial high-rates episodes: fact or fiction?
Cardiac implantable electronic devices (CIEDs) with atrial-lead
sensing afford clinicians a unique opportunity for continuous
heart-rhythm monitoring and the detection of atrial high-rate
episodes (AHREs). AHREs are recorded as atrial electrograms
(EGMs) and stored by CIEDs (date, number and duration of
these episodes are recorded). In this issue of the journal, Simu
and colleagues (page 102) have written an excellent review to
guide physicians and cardiac technologists who are faced with
interpreting and managing this relatively new entity.
1
Several
aspects of this review need to be highlighted.
Clinicians need to be aware of the definition regarding timing
and duration of an AHRE. The current 2020 European Society
of Cardiology atrial fibrillation guideline defines AHRE as
an atrial rate ≥175 beats per minute with a duration of at least
five minutes, while the European Heart Rhythm Association
(EHRA) consensus statement refers to higher atrial rates, > 190
beat per minute.
2-4
While the absolute atrial rate is not important, at these high
rates, AHREs are usually due to atrial fibrillation (AF), atrial
flutter or other atrial tachyarrhythmias. AHREs are usually
clinically silent, brief, and occur without a prior confirmed
diagnosis of AF or atrial tachycardia (AT). Paroxysmal episodes
of symptomatic AF, previously confirmed on a Holter or
electrocardiogram (so-called clinical AF), should not be classified
as an AHRE and have different clinical and management
implications as these patients are likely to have higher AF
burdens. The term subclinical AF can be also be used to describe
these AHREs in an asymptomatic patient and the terms can be
used interchangeably.
It must be noted that not all AHREs classified by the CIED
as AT or AF are due to AF or even an AT. This finding was
highlighted from the ASSERT (ASymptomatic atrial fibrillation
and Stroke Evaluation in pacemaker patients and the atrial
fibrillation Reduction atrial pacing) trial, which reported 17.3%
false positives when 6 000 AHREs were reviewed.
5
These
findings highlight the requirement that all EGMs be reviewed to
exclude false positives such as far-field oversensing of the T or R
waves, myopotentials, premature atrial ectopics, electromagnetic
interference on the atrial lead and other supraventricular
tachycardias. Examples of AHREs are shown in Figs 1 and 2.
As most patients are asymptomatic during AHREs, episodes
are often discovered incidentally at a routine pacemaker clinic.
Technologists and clinicians should always perform a detailed
CIED interrogation and review CIED diagnostics carefully to
classify AHREs. This is important as the incidence of AHREs
not due to AF is relatively high. In patients 65 years of age or
older without a prior history of AF, AHREs are detected in 10%
of subjects by three months of device implantation, in 24% by one
year and in 34% by two years.
6,7
If home monitoring is available,
downloads of transmissions must be reviewed on a regular basis. It
is important to emphasise that AHREs progress to clinical AF in
16% of patients over a 2.5-year period and should prompt closer
follow up of these patients, preferably with home monitoring.
6
There are still many unanswered questions with regard to the
clinical implications of AHREs. It is increasingly recognised that
AHREs are associated with an increased risk of stroke. However,
this finding comes mainly from the ASSERT trial, which was
the only trial that did not include patients with a prior history
of AF.
6
Therefore the burden of AF may have been higher in all
studies where prior clinical AF was recorded, with the finding that
AHREs (in the absence of prior clinical AF) increase the risk of
stroke, based on a single study. The lower burden of AF in patients
with AHRE/subclinical AF can explain the lower absolute
thromboembolic risk seen with AHRE compared to clinical AF.
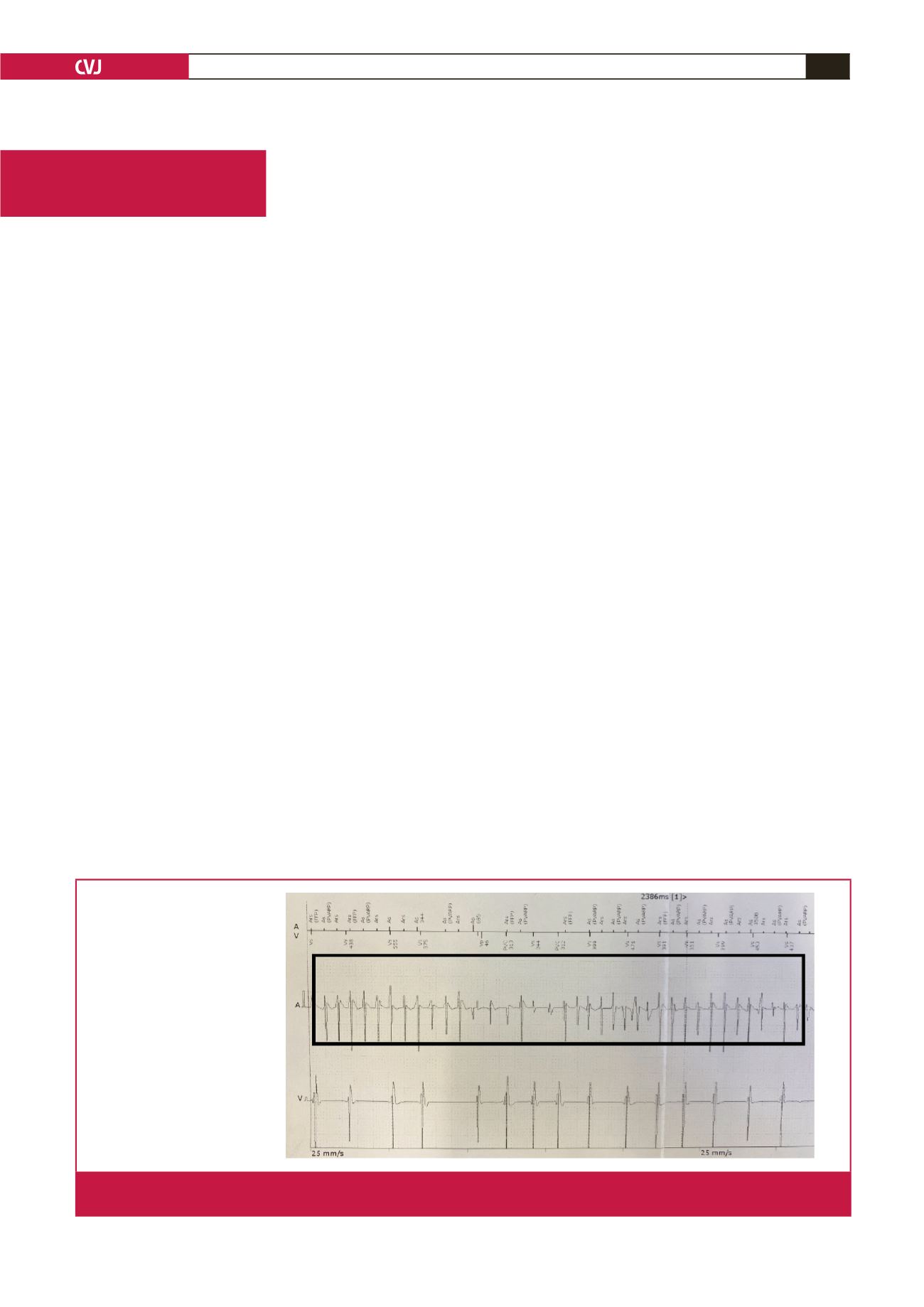
Atrial marker channel
Atrial EGM: A tip to ring
Ventricular EGM: RV tip to ring
Ventricular marker channel
Fig. 1.
Intracardiac EGMs and marker channels depicting an AHRE consistent with AF. The box indicates bipolar sensing of the
atrial lead with irregular fast atrial EGMs indicative of AF.



















