
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
72
AFRICA
were analysed. Descriptive statistics were used to analyse the
demographic data, disease characteristics, LSM compliance
and incidence of depression. The prevalence of depression was
established, and predictors of depression were determined using
multivariate analysis.
The results for all the variables were compared before and
after initiating LSM. The chi-squared test was used to determine
the association between disease characteristics and outcome
variables (depression and PA) at baseline and after LSM among
CABG and PCI patients. A general linear model was used to
evaluate the mean and standard deviation (SD) values, and the
differences between the group outcomes (depression severity
and number of subjects with depression) at baseline and after
three months of LSM, as a function of the main effect (group
differences). The changes in study outcome values (depression
and LSM compliance) from baseline to the final visit were
expressed in both the CABG and PCI groups.
Results
During recruitment, four patients were excluded due to severe
congestive cardiac failure (
n
= 3) and debilitating CVA (
n
= 1).
One hundred patients were recruited (58 males and 42 females),
and of these there were five dropouts who did not appear for
follow up after the three months of LSM, leaving 95 patients for
complete analysis at the end of the study.
The mean age of the participants was 60.56 ± 4.09 years,
with males and females having mean ages of 60.73 ± 4.52 and
60.29 ± 3.64 years, respectively. The ages of males and females
were normally distributed (
p
= 0.667 and
p
= 0.794, respectively)
(Shapiro–Wilk score = 0.829). The sample comprised mainly
Indians (73.0%), the remaining 27.0% being almost evenly split
among the other race groups.
Most of the patients were low- (53.0%) or moderate-income
earners (40.0%). Nine patients (9.0%) had a background history
of depression prior to the cardiac event and 55 (55.0%) reported
significant alcohol use. All the patients had previously sustained
an MI and had angiographically confirmed CAD. Most patients
had multiple CAD risk factors and nearly half of the patients
[48 (48.0%)] had at least one co-morbidity, the commonest being
chronic kidney disease (43.0%) (Table 1).
The overall prevalence of depression and depressive traits in
this sample was 51.0%. The main predictors of depression and
depressive traits were female gender (OR 3.29, 95% CI: 1.51–
11.03,
p
= 0.008), CABG (OR 1.86, 95%CI: 1.68–5.77,
p
= 0.003),
heart failure (OR 2.65, 95% CI: 5.87–13.62,
p
= 0.000), kidney
failure (OR 1.41, 95% CI: 1.30–5.23,
p
= 0.041), atrial fibrillation
(OR 1.60, 95% CI: 1.40–4.77,
p
= 0.023), low PA (OR 1.97, 95%
CI: 11.23–33.20,
p
= 0.000), previous history of depression (OR
8.99, 95% CI: 1.90–7.89,
p
= 0.002) and low income (OR 2.21,
95% CI: 1.40–2.85,
p
= 0.000). Level of education (OR 0.60, 95%
CI: 0.17–2.14,
p
= 0.430), age (OR 0.56, 95% CI: 0.71–2.00,
p
=
0.099), chronic obstructive pulmonary disease (OR 1.30, 95%
CI: 0.30–2.98,
p
= 0.327), as well as the other CAD risk factors,
complications and co-morbidities did not show any significant
influence on the outcome of depression (Table 2).
Prior to initiation of the LSM programme, five participants
(5.0%) were already physically active, six (6.0%) had changed
their diet on their own to a Mediterranean diet, and 11 (11.0%)
had stopped smoking cigarettes; however only three participants
(3.0%) were fully compliant with LSM
ab initio
. After three
months of the LSM programme, only 32 (33.7%) complied with
the protocol. Fifty-eight participants (61.1%) complied with the
dietary changes, 72 (75.8%) with cigarette smoking cessation and
38 (40.0%) complied with the minimum accepted PA (Table 3).
After the LSM intervention, the total number of subjects who
were physically active increased from five at baseline to 38 (40.0%)
three months later and the number who were insufficiently active
fell from 95% at baseline to 57 patients (60.0%) (both
p
= 0.000).
The PA score improved from 2.81 ± 4.410 at baseline to 11.65 ±
10.600 (
p
= 0.000) after LSM (Table 3).
At baseline, 51 participants (51.0%) had depression and
depressive traits and 49 (49.0%) were not clinically depressed
(36.0% had mild mood disturbance and 13.0% were
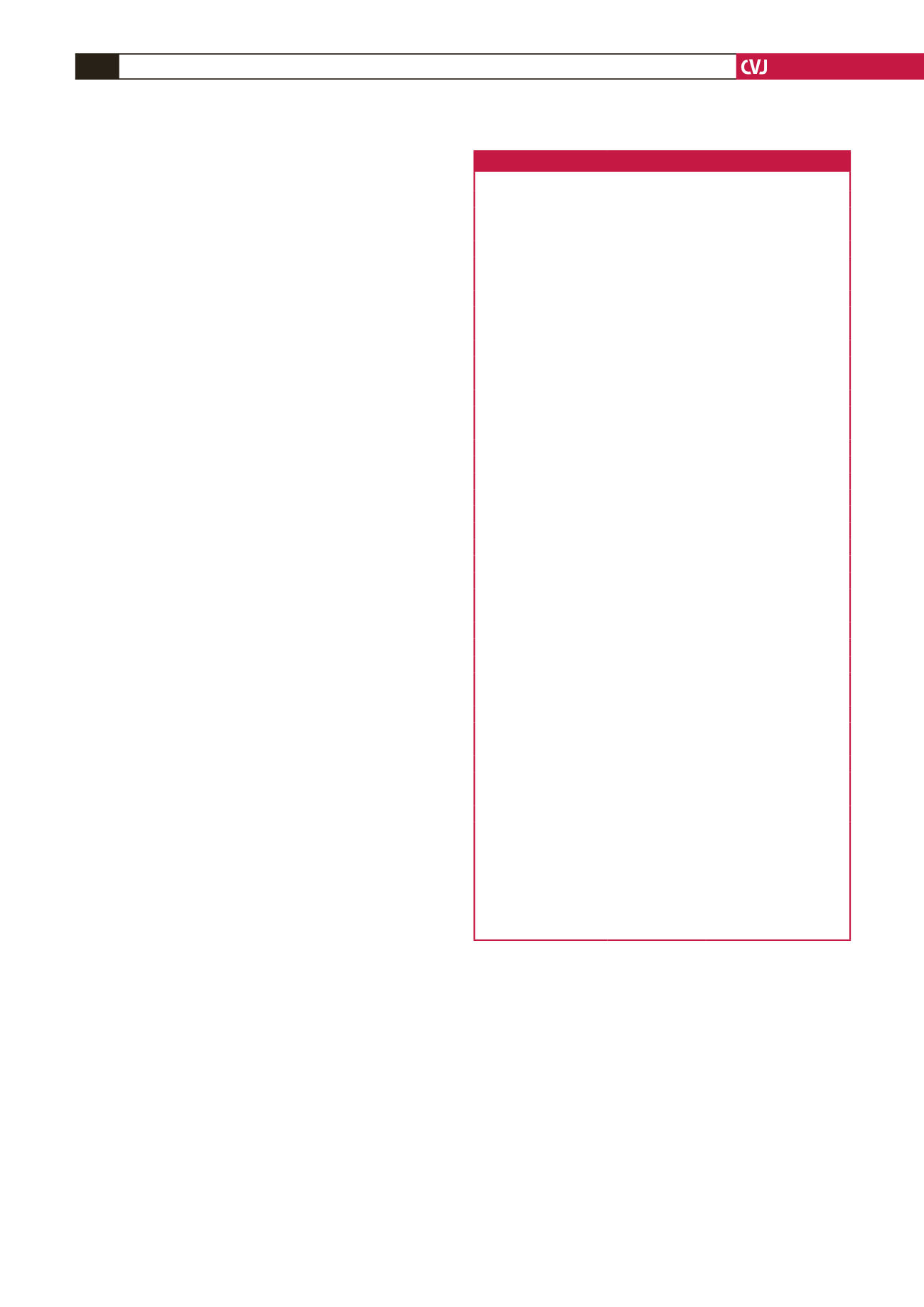
Table 1. Demographic data and baseline characteristics
Variables
Mean ± SD
Percentage (
n
= 100)
Age (years)
Male
60.73 ± 4.52
58.0
Female
60.29 ± 3.64
42.0
Race
Black
5.0
Coloured
8.0
Indian
78.0
White
9.0
Yearly income
Low
53.0
High/moderate
47.0
Educational level
Primary school
11.0
High school/tertiary
89.0
History of depression
Yes
9.0
No
91.0
CAD diagnosis
STEMI
89.0
NSTEMI
11.0
CAD risk factors
Hypercholesterolaemia
84.0
Diabetes
78.0
Hypertension
78.0
Sedentary lifestyle
76.0
Family history of CAD
53.0
Cigarette smoking
70.0
Obesity
45.0
Co-morbidities
Kidney disease
43.0
Arthritis
19.0
Other vascular diseases*
17.0
Hypothyroidism
7.0
COPD
4.0
Other co-morbidities
#
10.0
Complications
Heart failure
28.0
Atrial fibrillation
8.0
CAD: coronary artery disease; STEMI: ST-elevation myocardial infarction;
NSTEMI: non-ST-elevation myocardial infarction; COPD: chronic obstructive
pulmonary disease.
*Other vascular diseases: 11, peripheral vascular disease; six, cerebrovascular
accident.
#
Other co-morbidities: two, valvular heart disease; two, renovascular disease;
four, psoriasis; two systemic lupus erythematosus.
The sample comprised largely Indian subjects with multiple risk factors and
co-morbidities.



















