
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
AFRICA
73
psychologically normal). Among those with depression and
depressive traits, 18 (18.0%) had borderline depression, 23
(23.0%) moderate depression, and 10 (10.0%) severe depression
at baseline.
After the LSM intervention, the number of participants
with
depression and depressive traits fell from 51 (51.0%) to
33 (34.7%) (
p
= 0.022) and the number without depression and
depressive traits increased from 49 (49.0%) to 62 (65.3%) (
p
=
0.022) (Table 3). Of the latter group, 11 patients (17.7%) had
mild mood disturbance and 51 (82.3%) had no psychological
disturbance at all. Among the 33 who had depression post
LSM, 13 (39.4%) had borderline depression, 13 (39.4%) had
moderate, and seven (21.2%) had severe depression. The
mean depression scores fell from 21.91 ± 7.747 at baseline to
14.98 ± 9.610 (
p
= 0.002) after LSM, indicating a significant
reduction in the severity of depressive symptoms post LSM
(Table 3).
The severity and prevalence of depression and depressive
traits after the LSM intervention were compared in compliant
and non-compliant subjects. Both the depression severity and
the number of subjects with depression were significantly lower
in compliant subjects (both
p
= 0.000). Only one (3.0%) fully
compliant patient had depression compared to 32 (97.0%)
patients in the partly compliant group (
p
= 0.000) (Table 4).
Fifty-two patients underwent CABG [males 27 (51.9%);
females 25 (48.1%)], and 48 patients had PCI, [(males 31 (64.6%);
females 17, (35.4%)]. The mean ages in these groups were similar
and normally distributed (
p
= 0.140)
Most of the 95 (95.0%) participants were insufficiently active
at baseline, with only five (5.0%) being physically active. After
LSM the number who reached the desired PA level increased
from five (5.0%) at baseline to 38 (40.0%) (
p
= 0.000) three
months later. The PA score improved from 2.81 ± 4.410 at
baseline to 11.65 ± 10.600 (
p
= 0.000) after LSM (Table 3).
The PA scores were low for both the CABG and PCI groups
at baseline, although slightly higher for PCI (2.15 ± 4.160 and
3.53 ± 4.603, respectively) (
p
= 0.119). After 12 weeks of the
LSM regime, more patients undertook PA in the PCI group
compared to the CABG group: 27 (61.1%) versus 15 (33.9%)
patients participated often, seven (73.9%) versus two (21.1%)
sometimes, and 11 (23.7%) versus 33 (71.3%) rarely (
p
= 0.012).
The mean PA scores were also higher in the PCI compared to
the CABG group (14.16 ± 9.73 vs 9.40 ± 10.94, respectively) (
p
= 0.024). At the end of the study, 24 (60.0%) subjects in the PCI
group and 14 (35.0%) in the CABG group reached a satisfactory
level of PA based on the GLTE questionnaire cut-off points (
p
= 0.012).
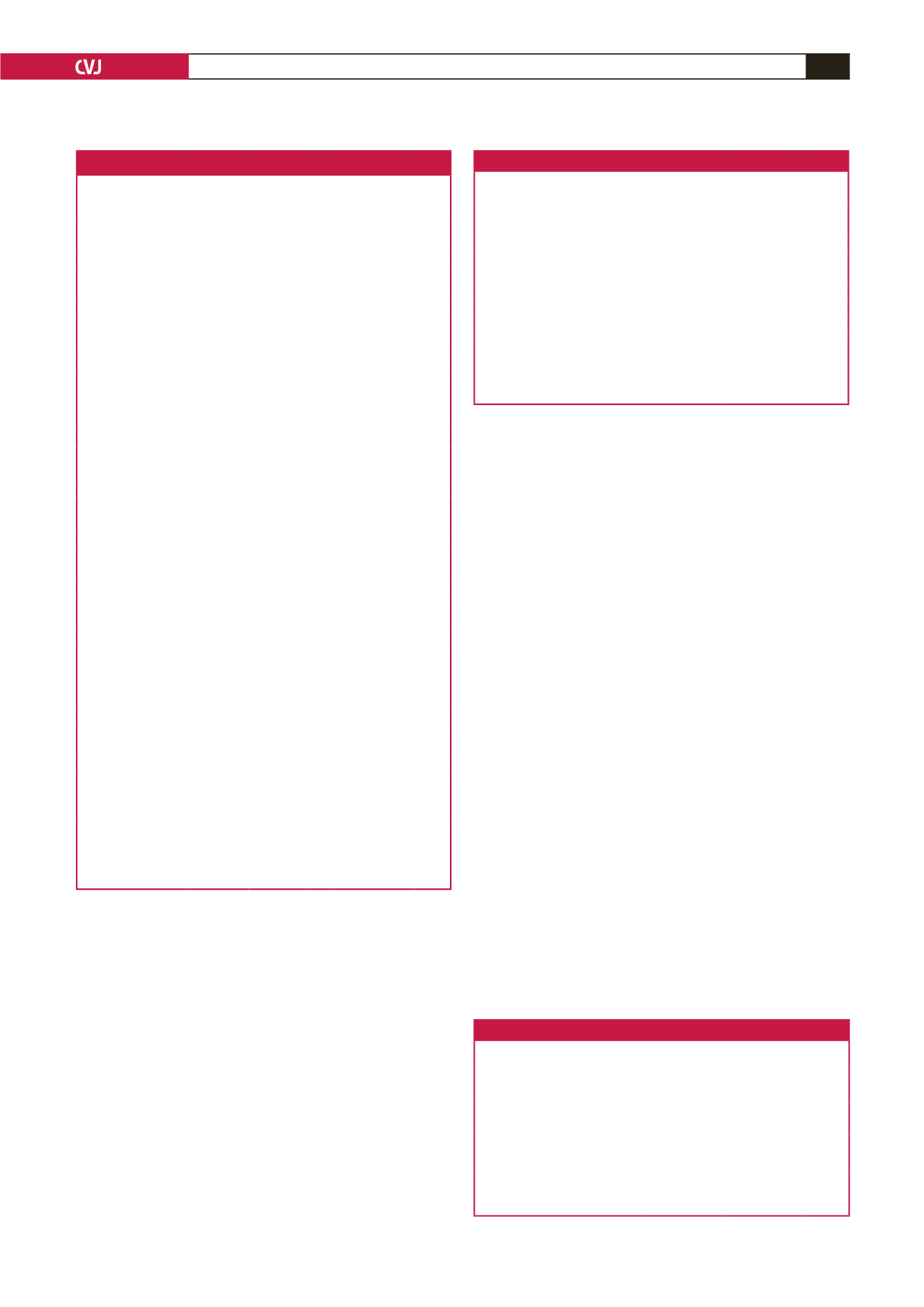
Table 3. Effects of LSM on lifestyle parameters and depression
Variables
Pre LSM
(n = 100)
Post LSM
(n = 95)
p-value
Aerobic exercise compliance,
n
(%)
5 (5.0)
38 (40.0)
0.000
Cessation of smoking,
n
(%)
11 (11.0)
72 (75.8)
0.000
Dietary modification,
n
(%)
6 (6.0)
58 (61.1)
0.004
Total LSM compliance,
n
(%)
3 (3.0)
32 (33.7)
0.000
Aerobic exercise score, mean ± SD 2.81 ± 4.41 11.65 ± 10.60 0.000
Depression score, mean ± SD
21.11 ± 7.75 14.98 ± 9.61 0.002
Depression,
n
(%)
51 (51.0)
33 (34.7)
0.022
No depression,
n
(%)
49 (49.0)
62 (65.3)
0.022
At the beginning, 100 patients were recruited, but there were five dropouts
during the study, leaving 95 participants for analysis after the LSM intervention.
Lifestyle modification yielded improved aerobic scores and a six-point reduction
in the depression scores, with a reduction in the incidence of depression after
LSM.
Table 4. Effects of LSM in compliant and partly compliant groups
Variables
LSM
compliant
LSM partly
compliant
p-value
Aerobic exercise score post LSM,
mean ± SD
15.94 ± 12.00 10.80 ± 9.80 0.018
Depression score post LSM,
mean ± SD
10.20 ± 7.00 16.70 ± 10.30 0.000
Depression,
n
(%)
1 (2.9)
32 (92.1)
0.000
No depression,
n
(%)
31 (47.5)
31 (47.5)
0.000
LSM: lifestyle modification yielded improved exercise scores and a fall in
depression scores with a reduction in the incidence of depression in compliant
subjects.
Table 2. Predictors of depression
Variables
Depressed
(n = 51)
No
depression
(n = 49) Total OR (95% CI) p-value
Age (years) mean ± SD 71 ± 1.122 71 ± 2.34
0.56 (0.71–2.00) 0.099
Gender,
n
(%)
Male
23 (45.1) 35 (71.4) 58 3.29 (1.51–11.03) 0.008
Female
28 (54.9) 14 (28.6) 42
Income,
n
(%)
Low
42 (82.4) 11 (22.4) 53 2.21 (1.40–2.85) 0.000
High
9 (17.6)
38 (77.6) 47
ACS intervention,
n
(%)
PCI
17 (33.3)
31(63.3) 48 1.86 (1.68–5.77) 0.003
CABG
34 (66.7) 18 (36.7) 52
History of depression,
n
(%)
No
42 (82.35) 49 (100) 91 8.99 (1.90–7.89) 0.002
Yes
9 (17.65)
0 (0)
9
Educational level,
n
(%)
Low
5 (9.8)
6 (12.2) 11 0.60 (0.17–2.14) 0.430
High
46 (90.2) 43 (87.8) 89
Physical activity,
n
(%)
Low
50 (53.0) 45 (47.0) 95 1.97 (11.23–33.20) 0.000
High
1 (20.0)
4 (80.0)
5
CAD risk factors,
n
(%)
Cholesterol
43 (84.3) 41 (83.7) 84 1.05 (0.36–3.06) 0.930
Diabetes
43 (84.3) 35 (71.4) 78 1.75 (0.79–5.70) 0.120
Hypertension
43 (84.3) 35 (71.4) 78 1.77 (0.80–4.50) 0.120
Sedentary life
39 (76.5) 37 (75.5) 76 1.05 (0.42–2.64) 0.910
Cigarette smoking 40 (78.4) 30 (61.2) 70 0.30 (0.80–1.60) 0.061
Obesity
27 (52.9) 24 (47.1) 51 0.95 (0.90–7.21) 0.567
Co-morbidities and
complications,
n
(%)
Kidney disease
27 (52.9) 16 (32.7) 43 1.41 (1.30–5.23) 0.041
Heart failure
24 (47.1)
4 (8.2)
28 2.65 (5.87–13.62) 0.000
Arthritis
11 (21.6)
8 (16.3)
19 1.41 (0.51–3.87) 0.504
Other vascular **
10 (19.6)
7 (14.3)
17 1.16 (0.71–4.21) 0.479
Thyroid disease
4 (7.8)
5 (10.2)
9 0.75 (0.19–2.97) 0.679
Atrial fibrillation
1 (2.0)
7 (14.3)
8 1.60 (1.40–4.77) 0.023
COPD
3 (5.9)
1 (2.0)
4 1.30 (0.30–2.98)
0.327
OR: odds ratio, ACS: acute coronary syndrome; COPD: chronic obstructive
pulmonary disease; PCI: percutaneous coronary intervention; CABG: coronary
artery bypass graft surgery.
Depression was commoner in women, those with a low income, kidney disease
and heart failure, and in those undergoing CABG compared to PCI.



















