
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 2, March/April 2021
74
AFRICA
At baseline, there were fewer PCI subjects with depression
compared to the CABG group [17 (33.3%) vs 34 (66.3%),
respectively (
p
= 0.047)]. The mean depression scores were lower
in the PCI group compared to the CABG group (19.20 ± 7.50
vs 22.10 ± 7.60) (
p
= 0.049), respectively, indicating more severe
depressive symptoms among CABG subjects at baseline (Table 5).
After three months of LSM, the number of participants
with depression and depressive traits fell from 51 (51.0%) to 33
(34.7%) (
p
= 0.022). Fewer cases of depression and depressive
traits were seen in the PCI compared with the CABG group
[8 (23.0%) vs 25 (72.0%) (
p
= 0.001)], respectively. There was a
corresponding increase in the number of non-depressed patients
in both groups, with a greater increment among the PCI subjects
[37 (56.7%) vs 25 (38.3%) (
p
= 0.001)]. The mean depression
scores followed the same pattern, with a greater score reduction
in the PCI compared to CABG group (7.90 vs 4.30, respectively)
(
p
= 0.000), suggesting that the PCI group derived greater benefit
than the CABG group from the LSM regime (Table 5).
After LSM, the prevalence of depression was significantly
lower among LSM-compliant subjects, with only one compliant
patient being depressed compared to 32 patients in the partly
compliant group (
p
= 0.001). Notably, the compliant CABG
and PCI patients derived nearly the same benefit from the LSM
programme (OR 1.10, 95% CI: 0.78–4.23,
p
= 0.191). There were
eight CABG and five PCI patients among the post-LSM fully
complaint patients with depressive traits at baseline (
p
= 0.125),
which reduced to one CABG and no PCI patient with depressive
traits post LSM (
p
= 0.063) (Table 6).
Discussion
In this prospective studywe evaluated the prevalence of depression
and depressive traits among MI patients after revascularisation
and analysed the effect of LSM on depressive symptoms. We
found a high prevalence of depression and depressive traits
(51.0%) among CAD patients who had sustained an MI and
undergone revascularisation. Similarly, several previous studies
have shown that depression is common among MI patients,
ranging from 10 to 65%.
1-7
Most of these studies were conducted
in developed countries, but a recent study by Ranjith
et al
.
analysed depression among MI patients in South Africa and
reported a prevalence of 49.0%.
29
In addition to evaluating the prevalence of depression among
these patients, we also analysed the effects of LSM on the
incidence of depression and compared the findings between
CABG and PCI patients. We found that LSM significantly
reduced both the incidence and severity of depression among
MI patients undergoing revascularisation, with compliant PCI
versus CABG patients deriving similar benefits. To the best of
our knowledge, no previous study has compared the effect of
LSM in these two categories of patients.
Many factors could have contributed to the high prevalence of
depression and depressive traits in our study, among them gender,
low income, previous history of depression, low PA, as well as
the presence of complications and other co-morbidities. Similar
to other studies,
16,19,29
we have shown that those participants with
a low income, previous history of depression and female gender
were more frequently associated with depression. In addition,
it appears those participants with more severe CAD requiring
CABG and the sicker patients (those with heart and kidney
failure) were more likely to experience depressive symptoms. This
is in contrast to the study of Pelletier
et al
., which showed that
disease severity did not influence the outcome of depression in
MI patients.
14
The high prevalence of depression in our study could also be
related to the fact that all our subjects had sustainedapreviousMI,
resulting in compensatory haemodynamic and neurohormonal
consequences of myocardial damage. Factors such as reduced
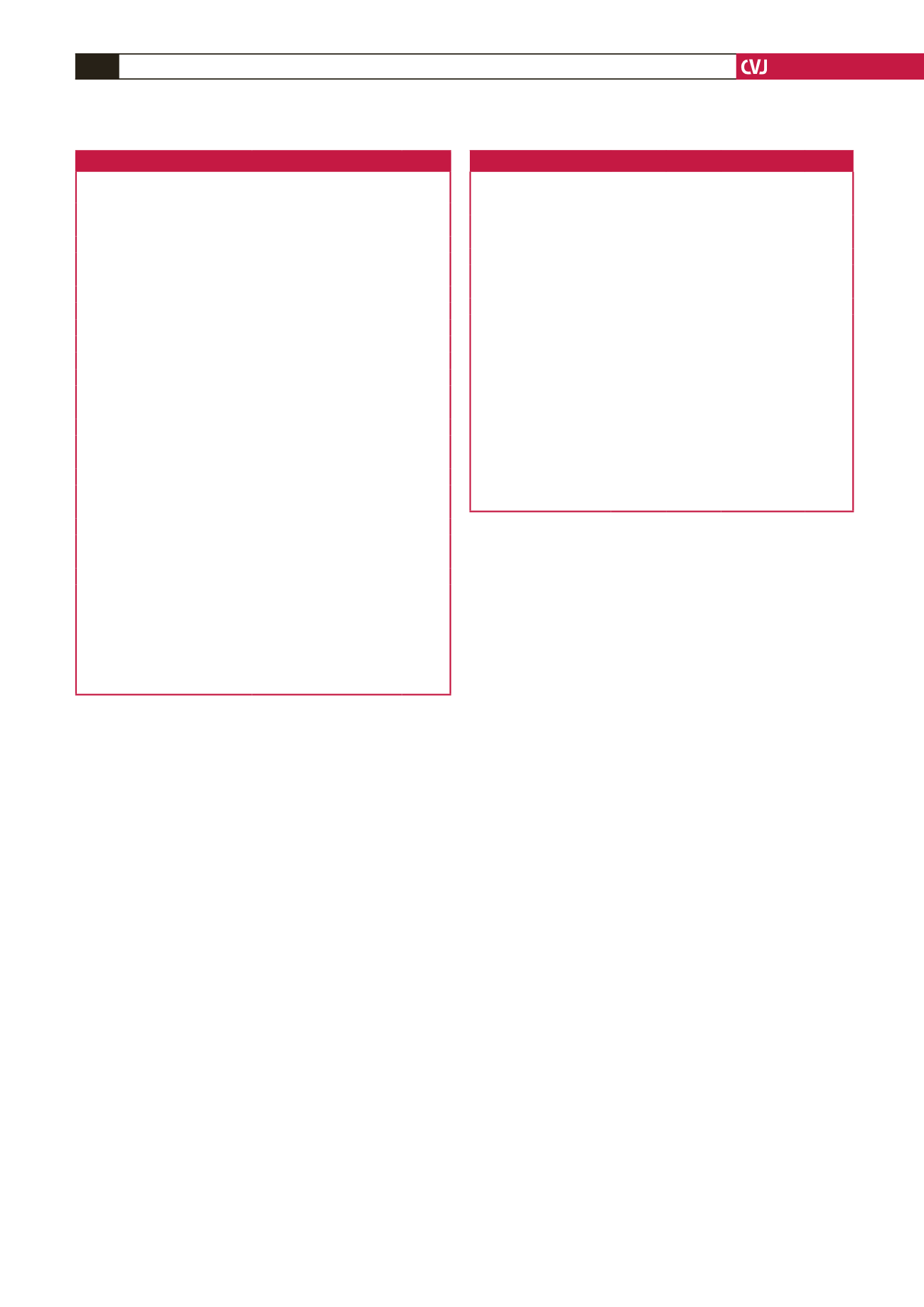
Table 5. Effect of LSM: CABG vs PCI group
Lifestyle parameters
CABG
(n = 52)
PCI
(n = 48) p-value
Aerobic exercise score, mean ± SD
Pre LSM
2.15 ± 4.16 3.53 ± 4.60 0.119
Post LSM
9.40 ± 10.94 14.16 ± 9.73
0.024
Aerobic exercise compliance,
n
(%)
Pre LSM
2 (40)
3 (60)
0.715
Post LSM
14 (35.0)
24 (60.0)
0.012
Dietary measures compliance,
n
(%)
Pre LSM
3 (50.0)
3 (50.0)
0.200
Post LSM
30 (49.1)
28 (45.9)
0.200
Smoking cessation compliance,
n
(%)
Pre LSM
6 (54.5)
5 (45.5)
0.590
Post LSM
40 (52.8)
32 (42.2)
0.593
Total LSM compliance,
n
(%)
Pre LSM
1 (33.3)
2 (66.7)
0.217
Post LSM
12 (35.6)
20 (59.4)
0.022
Depression score,
n
(%)
Pre LSM
22.10±7.60 19.20±7.50
0.049
Post LSM*
17.80±10.60 11.30±6.60
0.000
Depression status pre LSM,
n
(%)
Depressed
34 (66.7)
17 (33.3)
0.047
0.047
Not depressed
18 (36.7)
31 (63.3)
Depression status post LSM,
n
(%)
Depressed
25 (72.0)
8 (23.0)
0.001
Not depressed
25 (38.3)
37 (56.7)
0.001
LSM: lifestyle modification; PCI: percutaneous coronary intervention; CABG:
coronary artery bypass graft surgery.
LSM was more effective after PCI, with lower depression scores and reduced
incidence of depression, as well as improved aerobic and dietary compliance in
PCI subjects.
The lower participant numbers reflect the changes recorded in 95 participants
after LSM because there were five dropouts.
Table 6. Effects of LSM: compliant CABG vs compliant PCI groups
Variables
Compliant
CABG
(n =2)
Compliant
PCI
(n = 20)
OR
(95% CI)
p-value
Total LSM compliance,
n
(%) 12 (35.6) 20 (59.4) 1.70 (2.30–5.67) 0.022
Aerobic exercise score
14.96
18.91 1.10 (1.31–4.82) 0.049
Depression score
10.81
7.62 1.21 (1.12–3.92) 0.046
Depression pre LSM,
n
(%)
5 (41.7)
8 (40.0) 0.91 (0.89–3.97) 0.125
Depression post LSM,
n
(%)
1 (7.9)
0 (0.0) 0.96 (0.80–3.30) 0.063
No depression pre LSM,
n
(%) 7 (58.3) 12 (60.0) 1.0 (0.91–2.94)
0.097
No depression post LSM,
n
(%) 11 (87.1) 20 (95.0) 1.19 (0.75–4.10) 0.113
The prevalence of depression fell from five persons pre LSM to one post LSM
(80.0% reduction) among the fully compliant CABG group.
There was no person with depression post LSM, from the initial eight depressed
subjects (100.0% reduction), among the fully compliant PCI group.
The differences in reduction between fully compliant CABG and PCI patients
were 80.0 vs 100% (OR 1.10, 95% CI: 0.98–4.23,
p
= 0.191), which was not statis-
tically significant.
The number of patients with no depression increased from seven persons pre
LSM to 11 post LSM in the fully compliant CABG group (57.1%).
There was a 66.7% increment in the number of subjects with no depression post
LSM, from the initial 12 to 20 patients among the fully compliant PCI group.
The difference in increment between the fully compliant CABG and PCI groups
was 57.1 vs 66.7% (OR 0.91, 95% CI: 0.97–3.23,
p
= 0.210), which was not statisti-
cally significant.



















