
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 4, July/August 2021
AFRICA
225
which meant that the lesion had a greater microvascular blood
volume (Fig. 2B). Based on its location, appearance and
microperfusion, the diagnosis of a benign cardiac tumour (most
probably papillary fibroelastoma) was made.
Surgery was performed and it showed that a solid, mixed
cystic mass, originating from the posterior leaflet of the mitral
valve, approximately 20 mm in length, protruded into the left
atrium. The mitral valve mass was resected, while further intra-
operative transoesophageal echocardiography revealed severe
mitral regurgitation. An Edward bioprosthetic valve (25#) was
imbedded. The patient’s recovery was uneventful.
A postoperative pathological examination revealed that the
mass was a mitral valve myxoid change with calcification
(Fig. 3).
Discussion
CCMA, also called liquefaction necrosis,
2
is a rare type of mitral
annular calcification that describes chronic degenerative changes
of the cardiac fibrous skeleton, and mainly involves the area
between the crest of the posterior left ventricular muscle and the
posterior mitral annulus.
3,4
The elderly female population is the
most vulnerable although no clinical significance has been found
at present.
5,6
CCMA comprises a calcified rim and surrounding caseous
material that is composed of calcium, fatty acids and cholesterol,
with a toothpaste-like texture. Under the microscope, the
CCMA manifested as an amorphous, acellular, basophilic and
calcific structure, with a chronic inflammatory response with
macrophages as the most numerous cell type.
7
CCMA usually
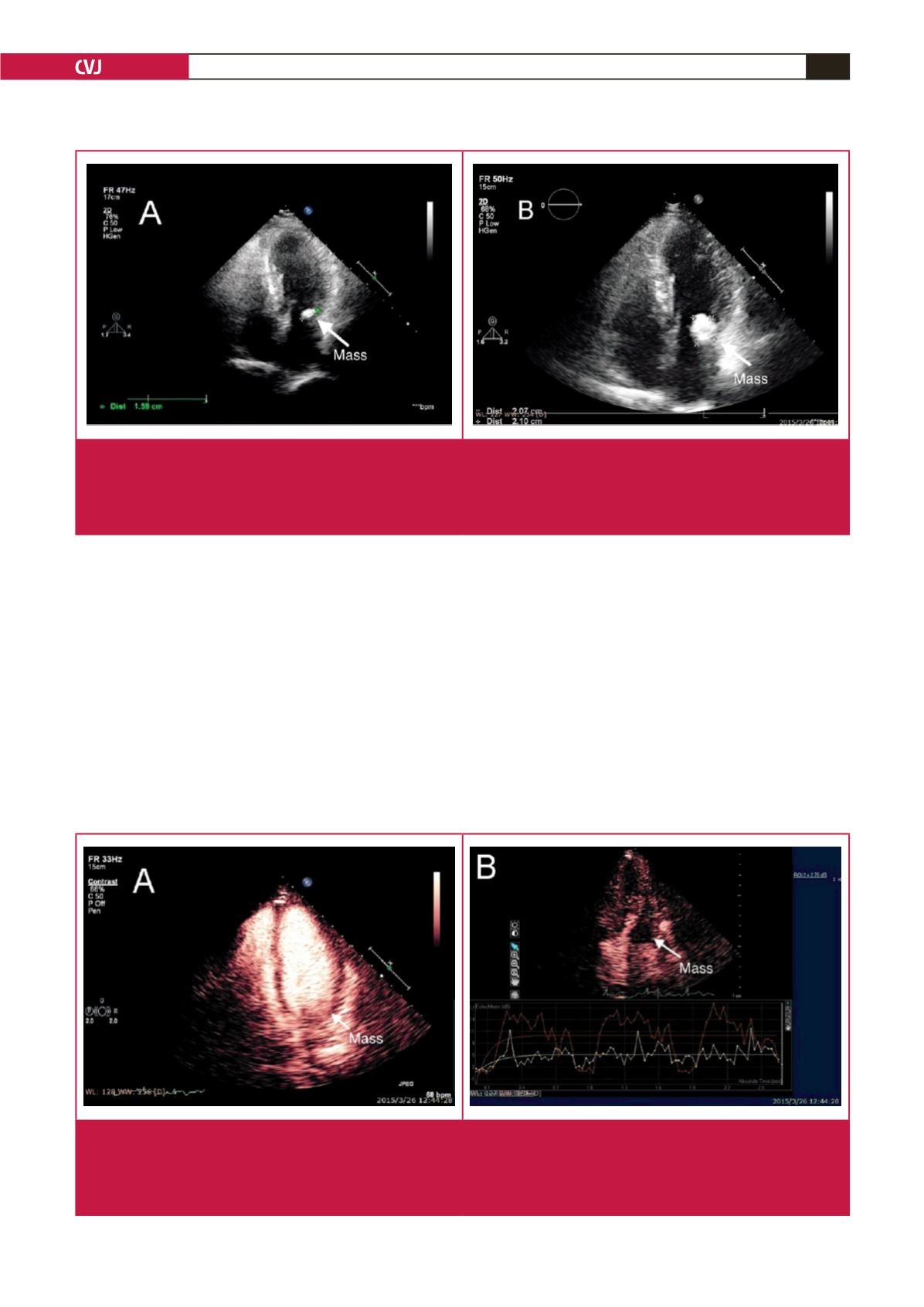
Fig. 1.
Echocardiographic images revealing the progression of the lesion. A. The mass was first incidentally detected by echocar-
diography four years earlier. The small, strong echo was limited to the mitral annulus like a calcified plaque. The size was
15 × 9 × 8 mm. B. Echocardiographic image taken on admission to our hospital. Compared with the image four years earlier,
the mass had enlarged to 22 × 20 × 16 mm, occupied the mitral valve orifice, and was accompanied by a secondary mitral
stenosis.
Fig. 2. Perfusion of the mass evaluated by myocardial contrast echocardiography. A. The image revealed a ring-enhancement mass
with distinct borders that was attached to the posterior leaflet of the mitral valve. B. Quantitative analysis was performed, with
a time–intensity curve obtained by the software attached to the equipment. The red line is the perfusion curve of the mass
membrane above the yellow line, which is the perfusion curve of the normal myocardium. Compared with the surrounding
normal ventricular myocardium, the mass represented a greater microvascular blood volume.



















