CARDIOVASCULAR JOURNAL OF AFRICA • Vol 21, No 2, March/April 2010
AFRICA
99
study of matched survivors who were withdrawn from chronic
beta-blockade and the case–control study of matched survivors
who continued chronic beta-blockade, 27 controls were matched
on all three risk factors, and one control was matched for two
risk factors. The patient characteristics of the 14 cases withdrawn
from chronic beta-blockade and died are presented in Table 3. All
14 patients were withdrawn from chronic atenolol therapy.
The demographic, clinical, surgical and physiological data of
the cohorts were similar with the exception of a history of hyper-
tension, which was more frequent in the matched control group
of survivors withdrawn from chronic beta-blockade (Table 4).
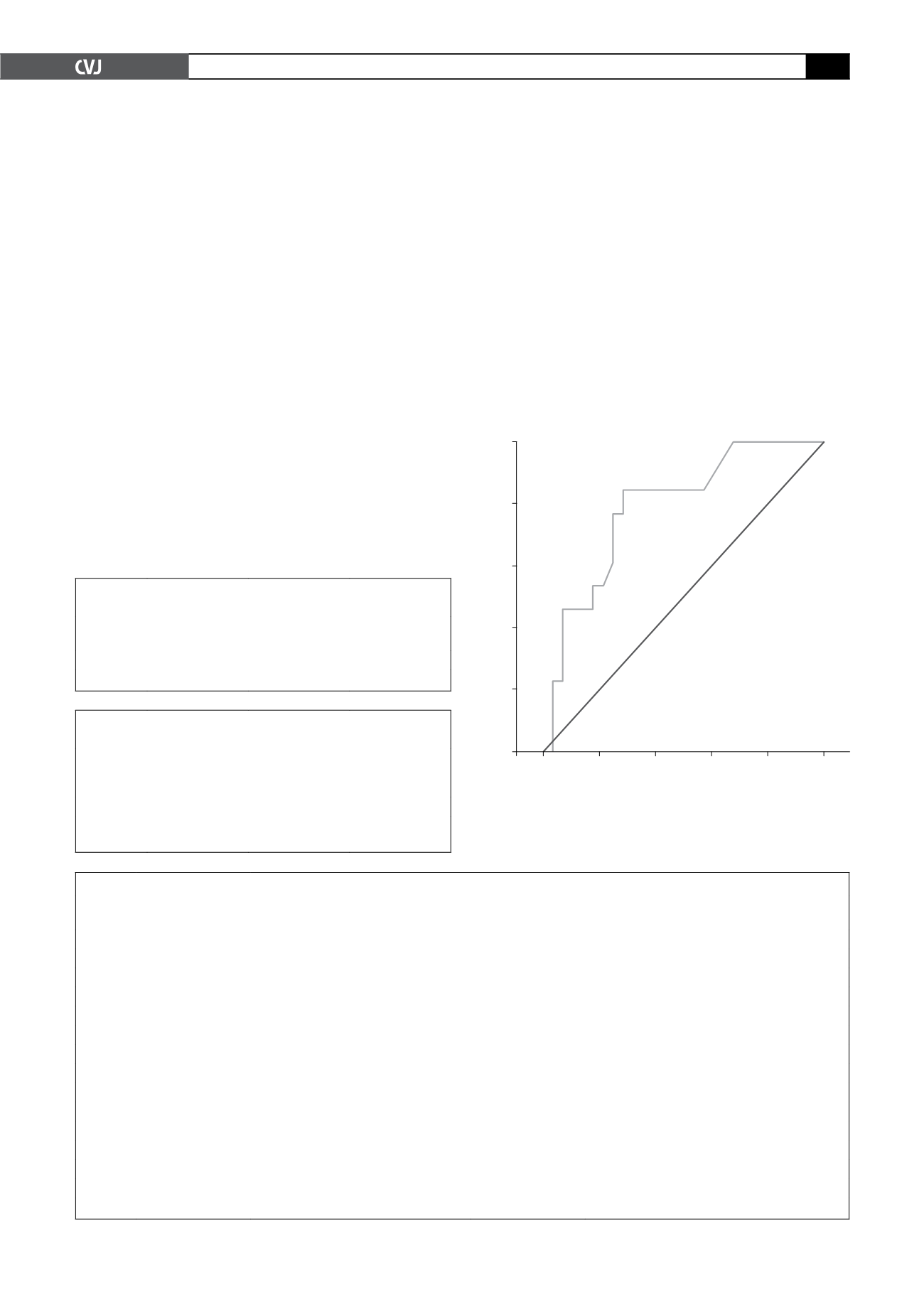
The conditional logistic regression identified that the post-
operative change in heart rate had the strongest association with
postoperative mortality in the matched cohort of withdrawn
survivors (Table 5). The ROC curve showed the optimal cut-off
point to be a mean increase in heart rate of
≥
six beats per minute
from the day of surgery to the ‘last mean daily heart rate’. This
had a sensitivity of 84.6% and a specificity of 71.4% and an
area under the curve of 0.787 (Fig. 1). For the cohort that was
maintained on chronic beta-blockade, the same cut-off point had
a sensitivity of 76.9% and a specificity of 65.4%. The area under
the curve was 0.778. The optimal cut-off point for this group was
a mean increase in heart rate of
>
5.8 beats per minute with an
84.6% sensitivity and 65.4% specificity.
No interaction was demonstrated between an increase in
heart rate of
≥
six beats per minute and non-administration of
beta-blockade within the first three postoperative days. Entering
both these variables into the multivariate analysis found only the
increase in heart rate to be independently associated with postop-
erative mortality following withdrawal of chronic beta-blockade
in vascular surgical patients (OR 13.7, 95% CI: 1.7–110,
p
=
0.014). In the case–control study of patients maintained on
chronic beta-blockade, neither the withdrawal of chronic beta-
blockade for all three postoperative days nor the increase in heart
rate were independent predictors of mortality. The heart rate
characteristics of the cases and controls of the case–control study
of patients withdrawn from chronic beta-blockade are presented
in Table 6.
TABLE 1. A HISTORY OF CHRONIC BETA-BLOCKADE
AND PER PATIENT IN-HOSPITAL MORTALITY
Chronic
beta-blockade
No chronic
beta-blockade
Odds ratio
(95% CI)
Mortality 28/195 (14.4%)
54/634 (8.5%) 1.80 (1.11–2.93)
CI: confidence interval;
p
=
0.02
TABLE 2.WITHDRAWAL OF CHRONIC BETA-BLOCKADE
AND PER PATIENT IN-HOSPITAL MORTALITY
Withdrawal
of chronic
beta-blockade
Administration
of chronic
beta-blockade
Odds ratio
(95% CI)
Mortality 21/108 (19.4%)* 6/86 (7.0%)
3.22 (1.24–8.38)
*The data on one death is excluded as this patient died intra-opera-
tively. CI: confidence interval;
p
=
0.01.
TABLE 3. PATIENT CHARACTERISTICS OF ‘CASES’WITHDRAWN FROM CHRONIC BETA-BLOCKADE
Patient
number
Postoperative days
withdrawn (
n
)*
Reason for withdrawal
of beta-blockade
Postoperative
day of death
Cause of death
1
1
Peri-operative inotropes
15
Cardiac: myocardial infarction
2
3
Unknown
26
Cardiac: cardiac arrest
3
3
Unknown
11
Non-cardiac: abdominal compartment syndrome
4
2
Unknown
2
Non-cardiac: cerebrovascular accident
5
1
Peri-operative inotropes
1
Non-cardiac: massive haemorrhage
6
3
Peri-operative inotropes
6
Cardiac: myocardial infarction
7
3
Unknown
8
Non-cardiac: respiratory failure
8
2
Unknown
2
Cardiac: myocardial infarction
9
1
Unknown
30
Cardiac: cardiac failure
10
1
Peri-operative inotropes
1
Cardiac: myocardial infarction
11
3
Unknown
3
Cardiac: myocardial infarction
12
3
Unknown
3
Non-cardiac: indeterminate
13
3
Postoperative ventilation
13
Non-cardiac: respiratory failure
14
3
Bradycardia
6
Cardiac: myocardial infarction
*Within the first three postoperative days
Fig. 1. The receiver operating characteristic curve for the
relationship between the increase in mean daily heart
rate following withdrawal of chronic beta-blockade and
in-hospital mortality.
1.0
0.8
0.6
0.4
0.2
0.0
0.0
0.2
0.4
0.6
0.8
1.0
Sensitivity
Specificity