CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 1, January/February 2011
32
AFRICA
88; 14.8%), and 2005–2007 (
n
=
64; 10.3%).
2,3
It is, however,
difficult to distinguish what is being reported when patients
are assessed to have died from cardiac, renal or respiratory
failure. Cardiac failure may lead to hypotension or pulmonary
oedema or both; renal failure implies fluid overload and there-
fore pulmonary oedema. Respiratory failure also carries the
inference of tachypnoea that may develop for many reasons,
including pulmonary oedema. It is likely that all these terms may
indicate deaths due to fluid overload, manifesting as pulmonary
oedema. If this is the case, then the total number of deaths due
to this cause exceeds the number of women dying from cerebral
events, and the number of such deaths has increased during the
most recent triennium, whereas the neurological mortality has
decreased.
Demographic data
Table 3 lists the age distribution and deaths due to hyperten-
sion. Of the 344 deaths from eclampsia, the majority occurred
in the age group below 34 years. However, there remains a large
proportion of deaths in the age group
≥
35 years. Most women
who die due to eclampsia and proteinuric hypertension are of low
parity, namely, 0 and 1.
Table 4 shows the percentage of total deaths per level of
healthcare due to hypertension. The concern is that although the
percentage of deaths may have declined at level one hospitals
over the years, the total number of deaths remains high. This may
be due to better reporting, but it probably indicates that patients
with hypertensive disorders are not being referred to higher
levels of healthcare timeously. This finding warrants a review of
referral protocols, or barriers to entry to higher levels of health-
care in the provinces. Similarly, the percentage of deaths at each
level of healthcare has not changed over the reporting periods.
Avoidable factors, missed opportunities and
substandard care
Table 5 shows the avoidable factors, missed opportunities and
substandard care for hypertension and gives a comparison with
the previous reports. There have been improvements in admin-
istrative factors but the emergency management of hypertensive
disorders remain a concern, particularly at level 1 hospitals.
Resuscitation problems have shown a slight decline.
Table 6 shows that there were no major differences in the
timing of the emergency event. It remains a concern that large
numbers of deaths are still occurring in the postpartum period. It
ought to be noted that many of the women categorised as having
had their emergency event in the postpartum period is arbitrary
because they actually had ante- or intrapartum complications,
with further complications in the postpartum period. However,
20 women had their first convulsion in the postpartum period,
either in hospital or at home following discharge from hospital.
Patient-orientated problems show slight improvements (Table
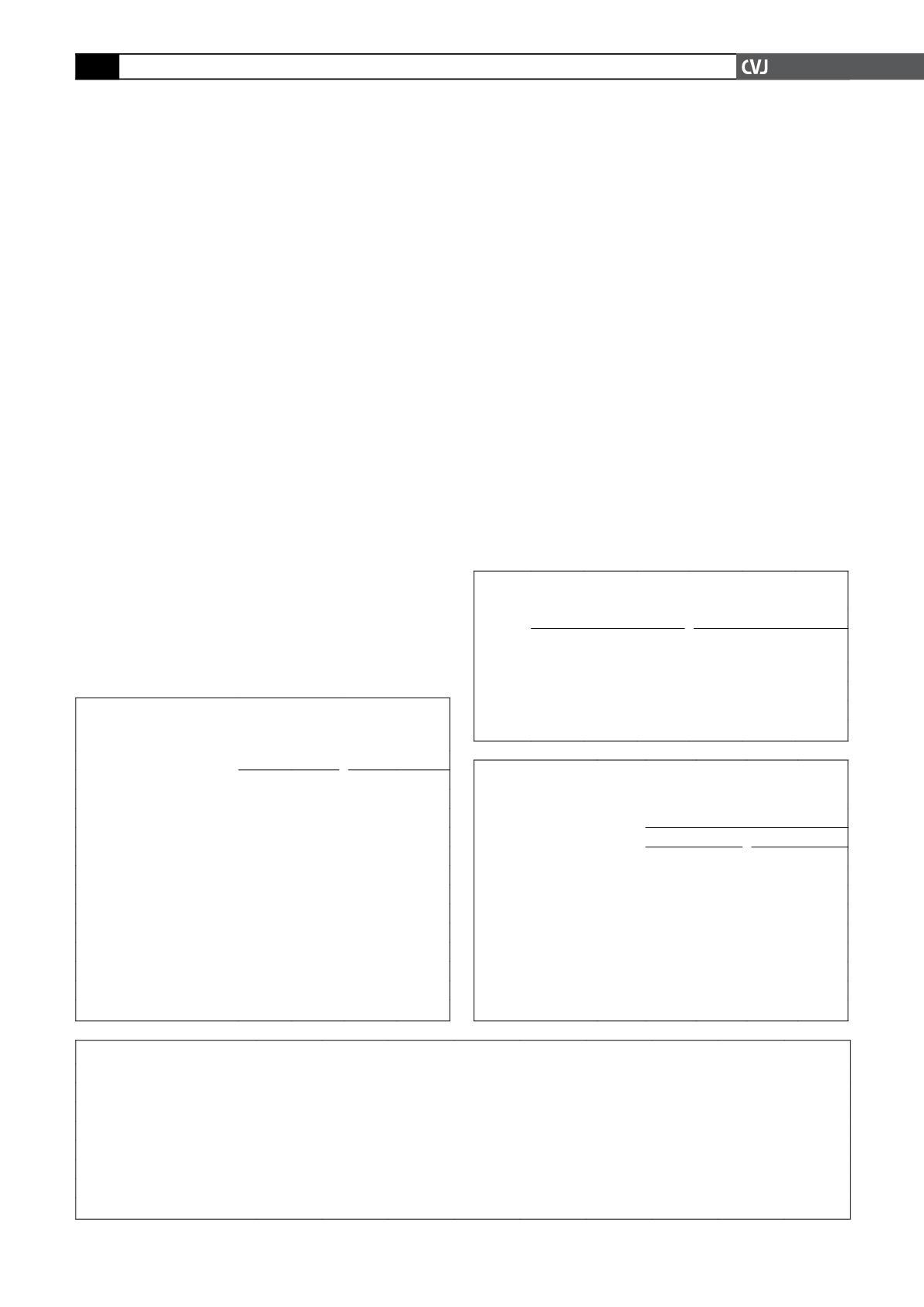
TABLE 2. FINALAND CONTRIBUTORY CAUSES OF
MATERNAL DEATHS FOR HYPERTENSIONANDA
COMPARISONWITH 2005–2007 AND 2002–2004
Organ system
2005–2007
2002–2004
n
%
n
%
Hypovolaemic shock
50
8.0
49
7.8
Septic shock
20
3.2
16
2.5
Respiratory failure
158 25.4 155 24.7
Cardiac failure
142 22.8
89 14.2
Renal failure
64 10.3
88 14.8
Liver failure
30
4.8
31
4.9
Cerebral complications
283 45.5 316 50.3
Metabolic complications
26
4.2
7
1.1
DIC
70 11.3
89 14.2
Multi-organ failure
88 14.1 104 16.6
Immune system failure
31
5.0
18
2.9
DIC: Unknown
56
9.0
56
8.9
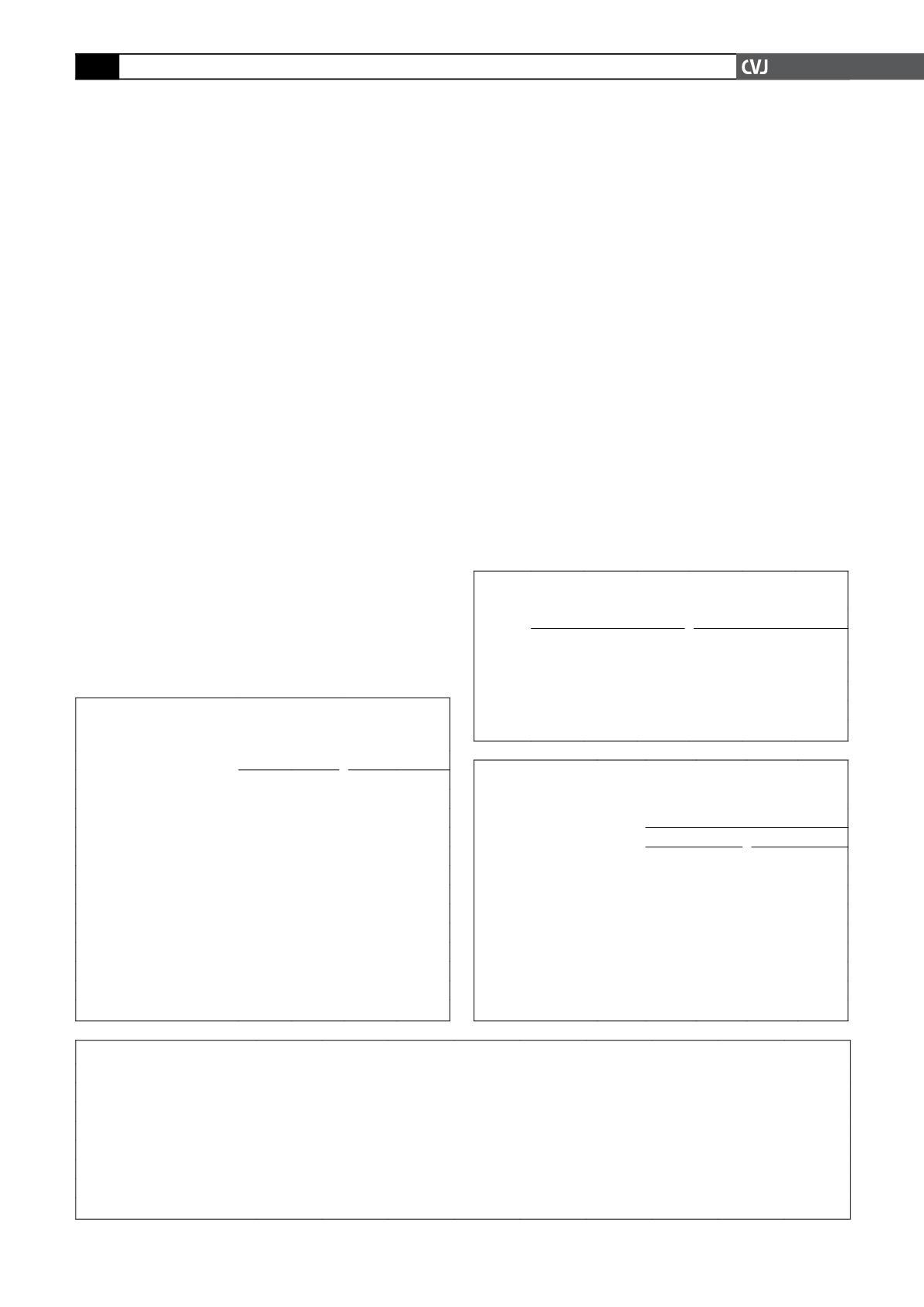
TABLE 3. AGE DISTRIBUTIONAND DEATH DUE TO HYPERTENSION IN PREGNANCY (YEARS)
Category
<
20
20–24
25–29
30–34
35–39
40–44
45
+
Unknown Total
Chronic hypertension
0
3
6
7
12
8
2
0
38
Proteinuric hypertension
19
43
33
44
21
11
2
0
173
Eclampsia
83
88
62
60
39
10
1
1
344
HELLP
6
10
13
14
7
4
0
0
54
Liver rupture
0
1
3
2
4
0
0
0
10
Acute fatty liver
0
0
3
0
0
0
0
0
0
Total
108
145
123
127
83
33
5
1
622
TABLE 4. PERCENTAGE OF TOTAL DEATHS PER LEVEL
OF HEALTHCARE CAUSED BY HYPERTENSION
Level
2005–2007
2002–2004
Total
deaths
HT
deaths
%
Total
deaths
HT
deaths
%
Level 1 1429 162 11.3 1103 149 13.5
Level 2 1527 232 15.2 1241 234 18.9
Level 3
850 202 23.8
941 233 24.8
HT: hypertension
TABLE 5. AVOIDABLE FACTORS, MISSED OPPORTUNITIES
AND SUBSTANDARD CARE FOR HYPERTENSIONAND
COMPARISONWITH 2002–2004
Category
Avoidable factors in assessable cases
2005–2007
2002–2004
n
% n
%
Patient orientated
232 42.4 250 47.7
Administrative factors
196 33.4 225 39.3
Health-worker orientated
Emergency
management
problems
Level 1 219 65.2 218 65.3
Level 2 117 34.8 149 51.7
Level 3 70 32
77 35.6
Resuscitation problems
136 24
148 27.5
Clearly avoidable deaths
=
304