CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 1, January/February 2011
AFRICA
33
7). It is well known that over 90% of women in South Africa do
have antenatal care but infrequent attendance and delay in seek-
ing help remain major issues.
Case 1
Management of severe hypertension in the
antenatal period
The patient, a 27-year-old parity 3, had high blood pressure
during her antenatal visits. She had had a previous caesarian
(C/S) and had three antenatal visits at a tertiary-care centre.
At her last visit, her blood pressure was 170/110 mmHg, she
was admitted at 11:00 and methyl dopa was prescribed. She had
a seizure at 23:00 on the day of admission. Magnesium sulphate
(MgS0
4
) was prescribed and a C/S was performed ‘under platelet
cover’. Post-operatively, there was difficulty in controlling her
high blood pressure; she had HELLP with jaundice and demised
at 12:00 the next day.
Lessons to learn: immediate management of severe
hypertension
Careful history taking and obtaining results of investigations is
essential. It is not clear whether information on her past obstetric
history was obtained. If she did have a previous C/S for hyper-
tension, laboratory results should have been obtained soon after
admission and appropriate action taken timeously. In this case
the results were only obtained following her seizure.
It is uncommon, for patients to ‘fit’ under medical manage-
ment in a tertiary hospital but this case illustrates the fulminant
course of pre-eclampsia that some patients develop. Therefore
all patients who are admitted with severe hypertension should be
treated with urgency.
•
Obtain a good past history.
•
Lower very high blood pressure reasonably quickly, but in
a controlled manner. Dihydralazine, if available, should be
used. Alternate antihypertensive agents include labetalol and
nifedipine.
•
All blood investigations must be reviewed within two to four
hours of being sent to a laboratory. This patient had low plate-
lets and HELLP probably on admission and it is likely that her
high blood pressure was not controlled.
•
Intensive monitoring of blood pressure levels must be
performed until they are stabilised.
Cases 2–4: postpartum convulsions
A 37-year-old delivered a premature baby at a MOU and was
transferred to a tertiary hospital because the baby required
level 3 care. The patient, on admission to the tertiary hospital,
complained of symptoms in keeping with imminent eclampsia
and had hypertension. The intern failed to make the correct diag-
nosis; therefore no observations were carried out. The next day
the patient was found in a post-ictal state and subsequently had a
cardio-pulmonary arrest.
A 23-year-old, parity 3 had a C/S for foetal distress and immi-
nent eclampsia. On the second post-operative day she developed
‘mild pulmonary oedema’. She responded to initial treatment;
12 hours later, she convulsed and had a cardio-pulmonary arrest.
A parity 1 G 2 had severe pre-eclampsia. She had a normal
vaginal delivery but was discharged on day 1 following delivery,
with no treatment. She ‘fitted’ at home 24 hours later and had a
cardio-pulmonary arrest.
Lessons to learn
These cases illustrate features of severe pre-eclampsia syndrome
that are often not taken into account by inexperienced health
personnel. While it is true that in our current understanding of
the aetiology of pre-eclampsia that delivery of the foetus and
placenta leads to cure, it must be understood that these women
are still at risk of complications from the disease process in
the immediate post-delivery period. Therefore it is essential to
ensure continued frequent observations of the pulse rate, blood
pressure, urine output, level of consciousness and potential signs
of pulmonary oedema.
Antihypertensive therapy must be continued and should not
be stopped abruptly. Magnesium sulphate should be continued
for at least 24 hours following delivery. All laboratory tests
must be repeated within four to six hours following delivery
and results reviewed. Patients should not be discharged until
their high blood pressure levels are stabilised for a period of at
least 24 hours. Furthermore, these patients should be asked to
return to the postnatal clinic within a week and only referred to
a clinic when all physical and laboratory tests have returned to
normal. Generally speaking, these tests should have returned to
normal within seven days of delivery. Advice on contraception,
further pregnancies and place of future antenatal care should be
provided.
All three cases illustrate the above lessons, namely
•
failure to recognise symptoms and signs of imminent eclamp-
sia following delivery and consequently failure of post-deliv-
ery observations
•
failure to recognise dangers of pulmonary oedema, the need
for investigations and frequent observations
•
discharging patients from hospital prior to stabilising (lower-
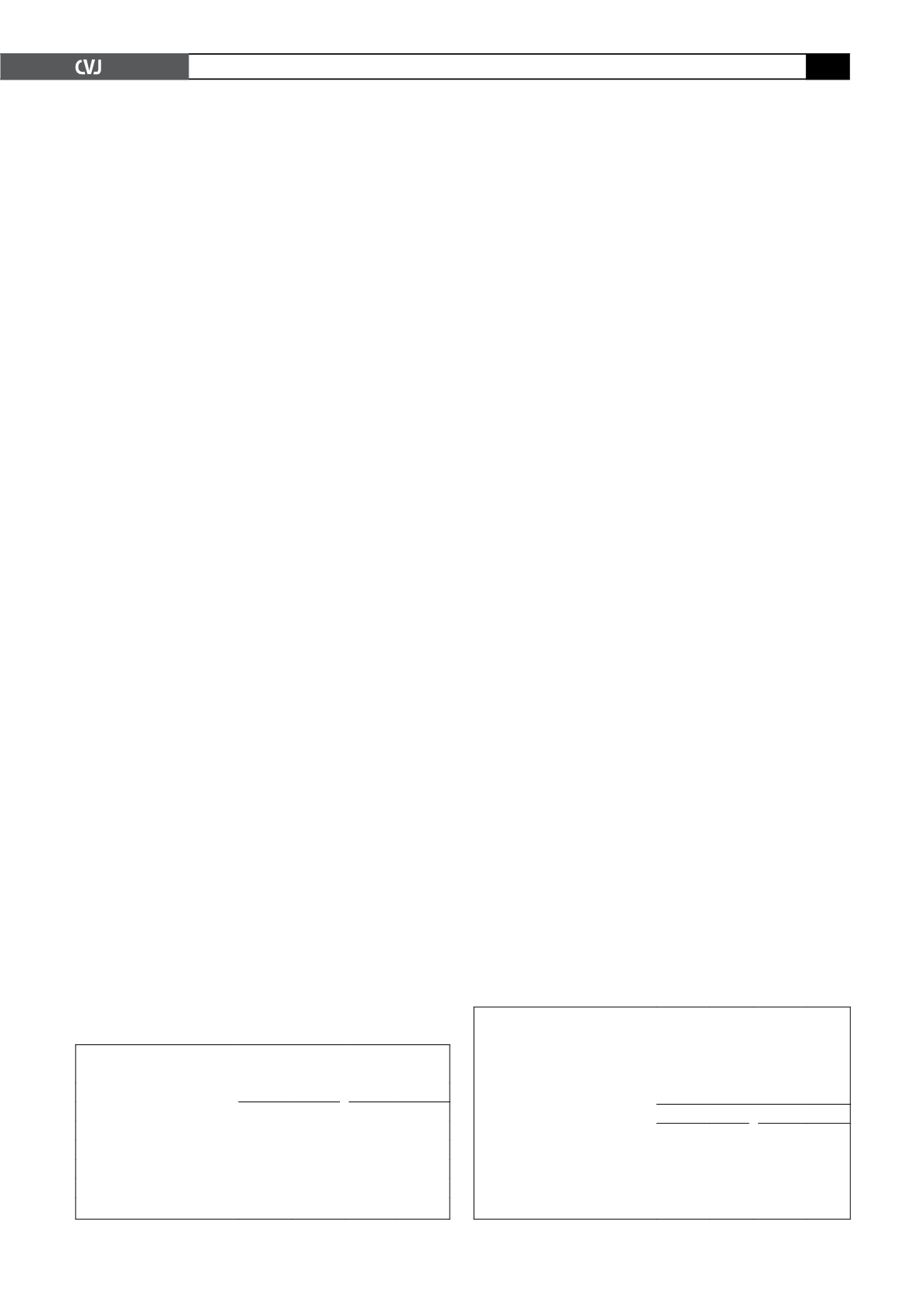
TABLE 6. TIMING OF EMERGENCY EVENT
RELATED TO HYPERTENSION
Category
2005–2007
2002–2004
n
% n
%
Early pregnancy
14
2.3
13
2.1
Antenatal period
335 53.9 206 48.7
Intrapartum
69 11.1
83 13.2
Postpartum period
209 33.6 228 36.3
Unknown
3
0.5
5
0.8
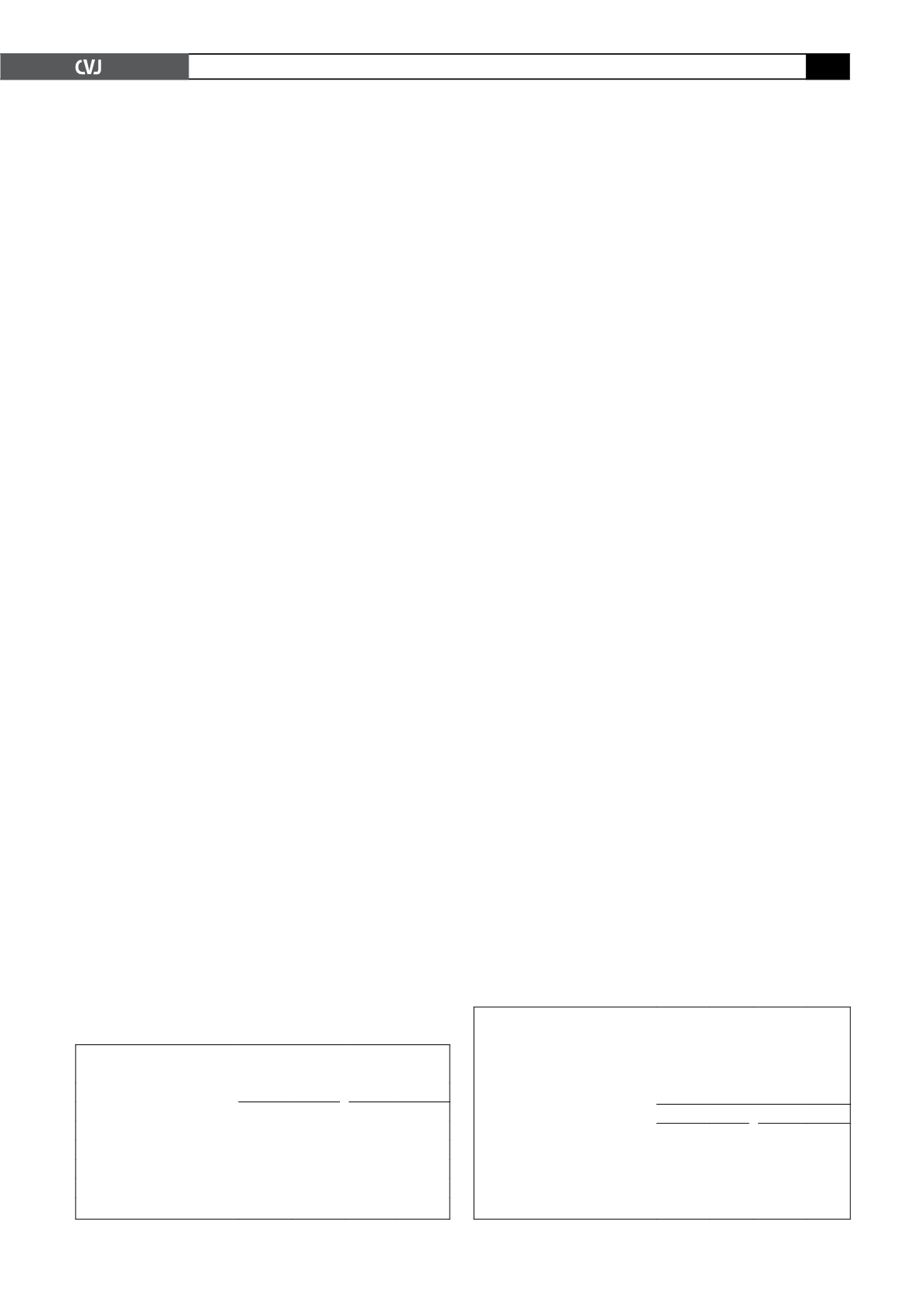
TABLE 7. AVOIDABLE FACTORS, MISSED OPPORTUNITIES
AND SUB-STANDARD CAREWITH RESPECT TO PATIENT-
ORIENTATED PROBLEMS FOR HYPERTENSIONANDA
COMPARISONWITH 2002–2004
Major problems
% of assessable cases with
avoidable factors
2005–2007
2002–2004
n
=
547 % n
=
524 %
Non-attendance of antenatal care 106 19.4 123 23.5
Infrequent attendance
40
7.3
36
6.9
Delay in seeking help
106 19.4 140 26.7
Other
45
8.2
38
7.3