CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 3, May/June 2011
132
AFRICA
gas exchange in our study setting. In an oleic acid-induced lung
injury model, it has been demonstrated that low concentrations
of isoflurane resulted in an increase in ventilation and perfusion
mismatch, as evaluated by multiple inert gas analysis.
26
However,
AaDO
2
in the injured lungs was not significantly changed by
inhalation of the low concentrations of isoflurane.
26
By contrast, in a porcine model with gas-exchange defect by
air pneumoperitoneum, it was shown that sevoflurane but not
isoflurane caused significant ventilation and perfusion mismatch
using the multiple inert gas elimination technique.
32
The differ-
ences between the experimental model (oleic acid-induced
vs air pneumoperitoneum-induced gas-exchange defect) and
the controls (sodium pentobarbital-anaesthetised animals with
definite lung injury vs propofol-anaesthetised animals with
gas-exchange defect) may account for the inconsistence shown
in the abovementioned two experiments regarding the effect of
isoflurane on gas-exchange disturbance.
It is well known that PMNs play a key role in the develop-
ment of post-CPB lung injury.
1-5,22
Previous studies showed that
volatile anaesthetics reduced PMN adhesion in the reperfused
coronary system.
33,34
Recently it was demonstrated that isoflurane
pre-treatment attenuated PMN accumulation in the lung inter-
stitium and alveolar space in a male mouse model of lipopoly-
saccharide-induced lung injury.
12
Our results of PMN counts
showed that isoflurane remarkably alleviated PMN filtration into
the non-dependent and dependent lung regions three hours after
declamping, indicating that isoflurane could be beneficial for
inhibition of inflammation in lungs during CPB.
Some limitations of our experiment should be noted. First,
pentobarbital showed an inhibitary effect on HPV.
35
Consequently,
the effects of isoflurane on CPB-related lung injury may be
altered with the pentobarbital anaesthesia. However, the results
should be reliable since a continuous quantitative infusion (25
mg/kg as an initial bolus and then 4 mg/kg/h) of pentobarbital
was performed in the current study. In addition, to prevent any
antegrade flow to the lungs and therefore make any lung injury
in each animal as similar as possible, our animals were subject
to pulmonary artery as well as aortic clamping during CPB. This
may have aggravated the degree of lung injury, in that exposure
to CPB alone is enough to cause pulmonary injury, and cessation
of pulmonary arterial flow during CPB contributes significantly
to pulmonary dysfunction.
24
Conclusion
The present study showed that 30-min pre-treatment with 1.0
MAC isoflurane before CPB alleviated PMN accumulation in
canine lungs, inhibited the increase in PVR, and did not signifi-
cantly affectAaDO
2
in the early post-CPB stage, suggesting isoflu-
rane could be beneficial in preventing CPB-related lung injury.
The authors thank Drs Xuejun Li, Wanfu Pen and Qiansu Chen, Department
of Cardiac Surgery, the Affiliated Hospital of Guiyang Medical College,
Guiyang, Guizhou, China, for their assistance in the establishment of some
procedures of CPB.
References
1.
Asimakopoulos G, Smith PL, Ratnatunga CP, Taylor KM. Lung injury
and acute respiratory distress syndrome after cardiopulmonary bypass.
Ann Thorac Surg
1999;
68
: 1107–1115.
2.
Dreyer WJ, Michael LH, Millman EE, Berens KL, Geske RS.
effusions.
25
Dogs pre-treated with isoflurane in our experiment
showed significantly reduced DLC values after CPB, as did
the control group. However, no difference in DLC was found
between the two groups. Consistent with our DLC results, in an
oleic acid-induced lung injury model, it was also documented
that lung compliance of the injured canine lungs was not affected
by inhalation of isoflurane.
26
In the present study we found 30-min pre-treatment with 1.0
MAC isoflurane before CPB significantly decreased PVR in the
early post-CPB stage. The effect of isoflurane on PVR shown
in our study may potentially be ascribable to the demonstrated
phenomenon that isoflurane attenuates hypoxic pulmonary
vasoconstriction (HPV).
27-30
It has been shown that metabolites
of the cyclooxygenase pathway,
28
endogenous vasodilator,
29
calci-
um-activated potassium (K
Ca
) channels and voltage-dependent
potassium (K
V
) channels
30
may be involved in the modulation of
isoflurane-induced attenuation of HPV. More recently, it has been
reported that TASK-1 channels play a role in HPV and contribute
to volatile anaesthetic-induced pulmonary vasodilation.
31
In our experiment, although it was striking that gas exchange
in the isoflurane group, assessed by AaDO
2
changes, dete-
riorated steadily following the diminution of PVR after aortic
declamping, no difference in AaDO
2
was found between the
isoflurane-treated and control groups. The reason might be that
the inhibition of HPV by isoflurane caused only minor effects on
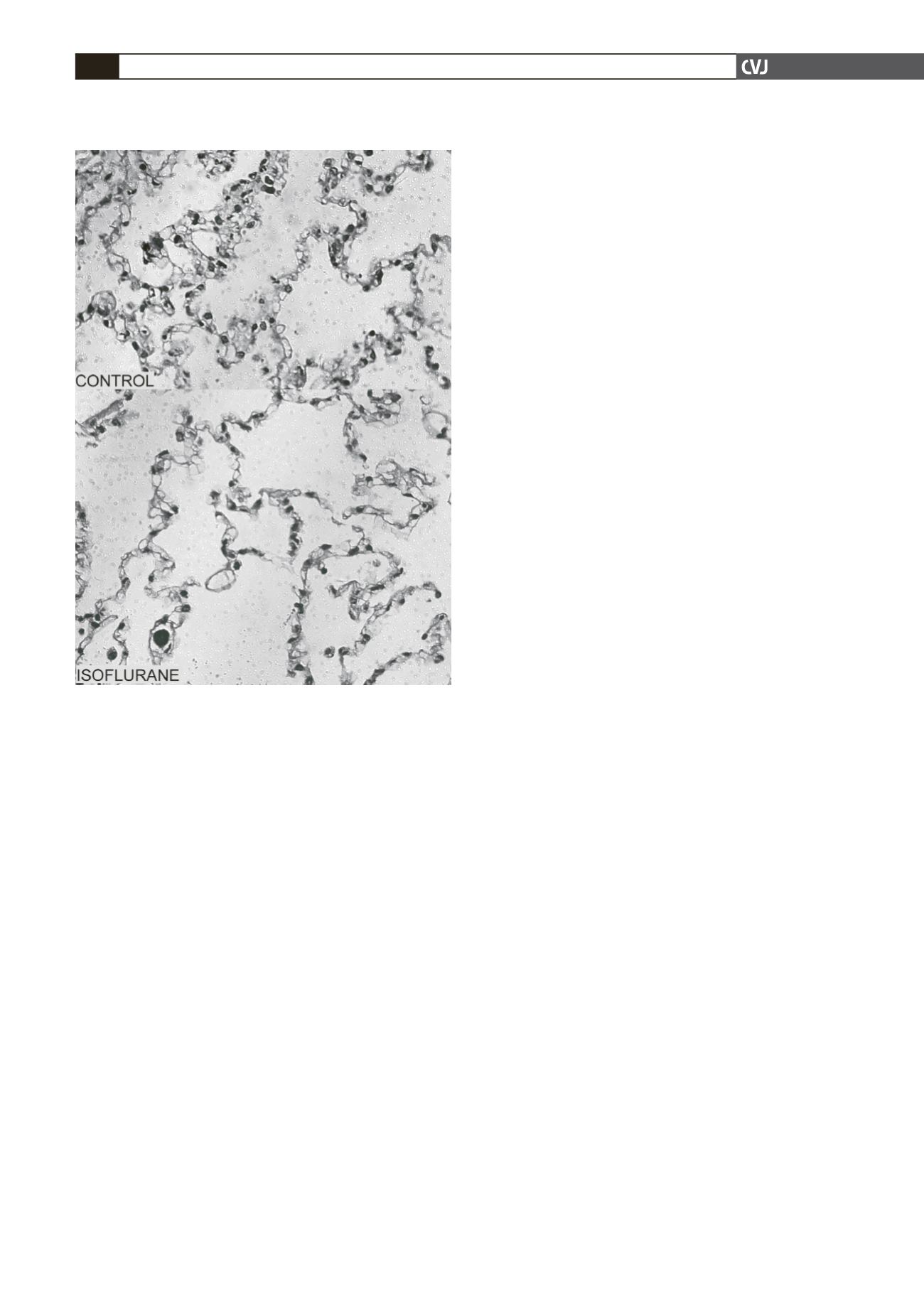
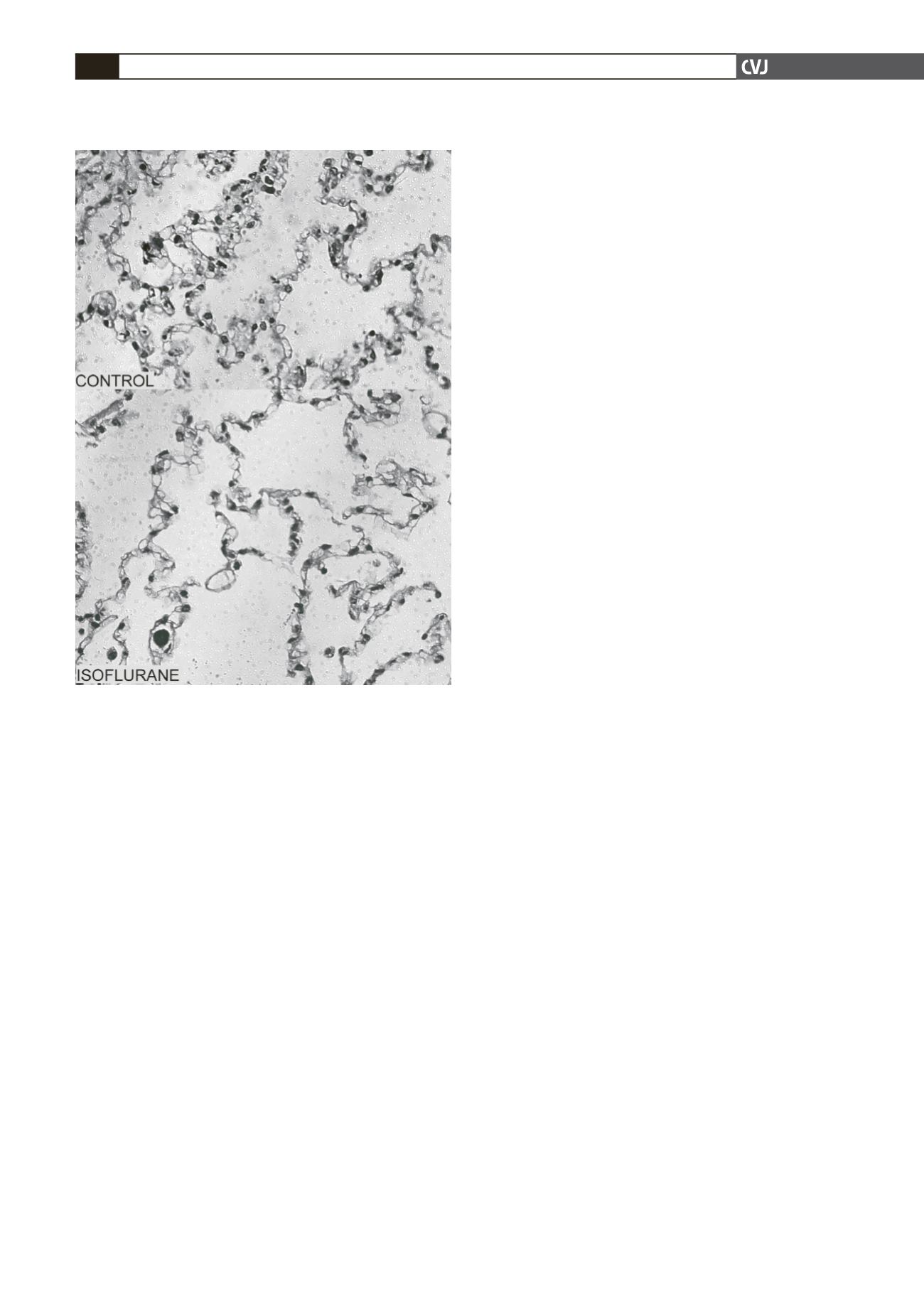
Fig. 3. Microscopic findings of polymorphonuclear leuko-
cyte (PMN) filtration in the dependent portion of the lower
lobe of the left lung three hours after aortic declamping in
the control and isoflurane groups (haematoxylin-eosin;
magnification
×
400).