CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 3, May/June 2011
142
AFRICA
physical examination was unremarkable.
The basic laboratory parameters were within normal limits.
MRI of his head and his EEG revealed no abnormalities. The
only significant finding was his ECG, which showed a Wolff–
Parkinson–White (WPW) pattern (Fig. 1). He had no record of
previous ECG. With this negative work up and normal neuro-
logical examination, the seizure episode was attributed to WPW
syndrome, leading to tachyarrhythmia and a transient haemo-
dynamic instability, which in turn would have caused cerebral
hypoxia leading to seizure.
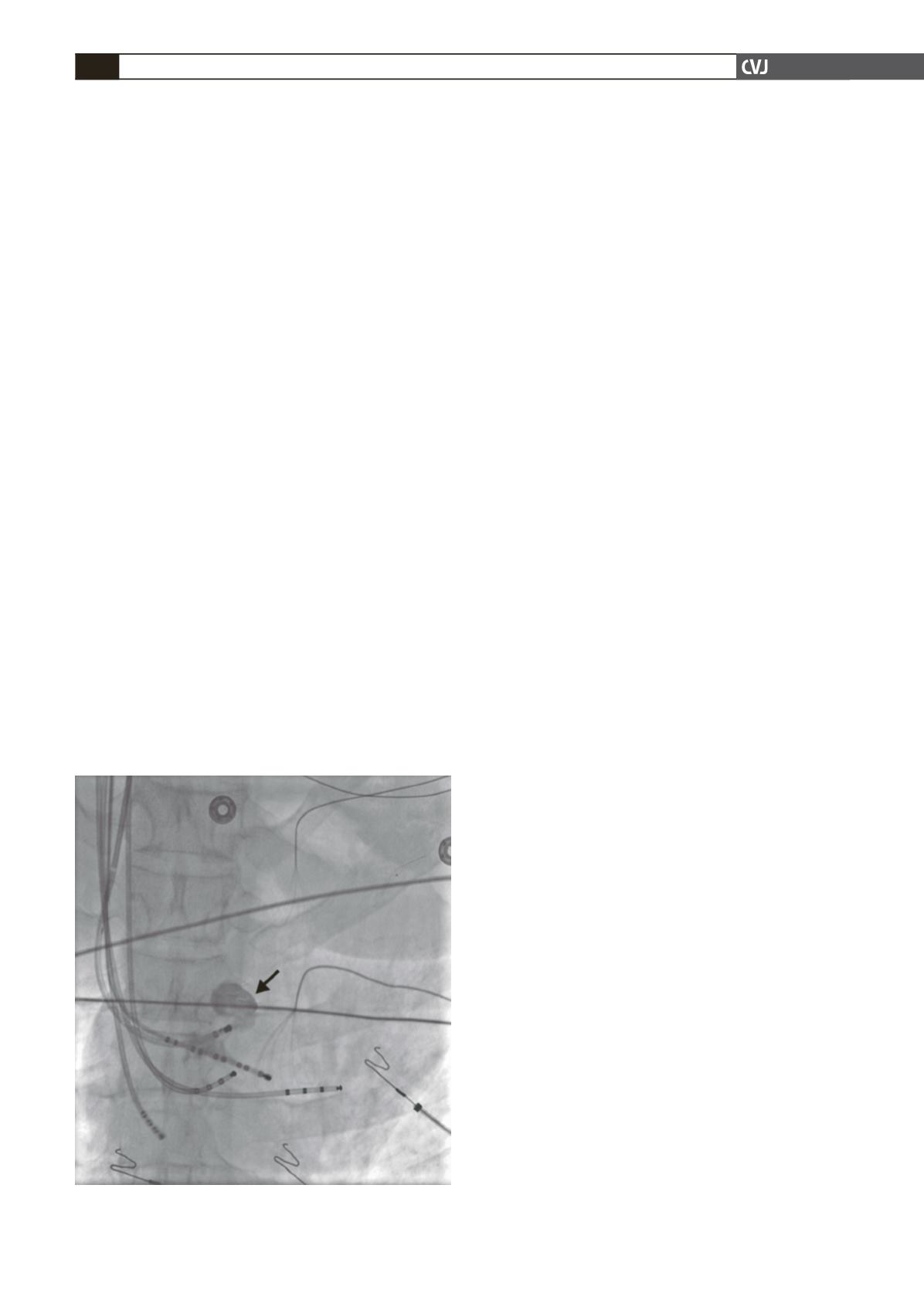
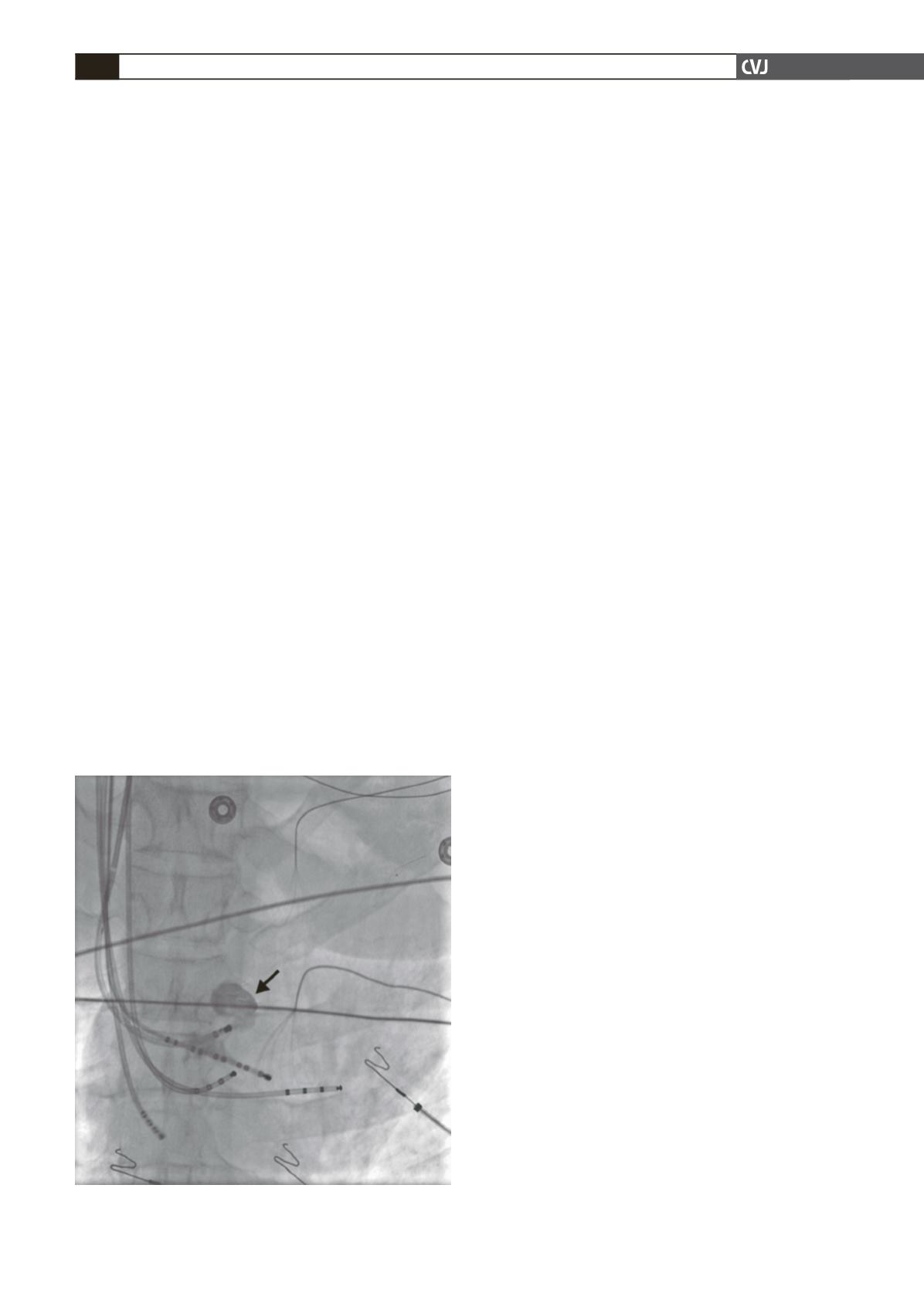
Further work up included a stress test and two-dimensional
echocardiogram, both of which turned out to be normal. He
was taken for cardiac catheterisation and electrophysiological
study (EPS), which revealed coronary sinus aneurysm (Fig. 2)
and an accessory pathway within the coronary sinus aneurysm.
Arrhythmogenicity was confirmed by inducible ventricular
fibrillation during EPS. Coronary sinus aneurysm was further
confirmed by CT angiogram.
Ablation of the aneurysm was warranted but the inaccessible
location within the coronary sinus proved to be a challenge.
Later, a probe was custom made for this purpose and the acces-
sory pathway was successfully ablated.
Discussion
Abnormalities in the coronary sinus are unusual and they may
coexist with accessory pathways. Their real incidence is not
known. In a recent report by Morgan
et al
.,
4
4% of 300 patients
with cardiac rhythm anomalies had a coexistent anomalous
coronary sinus.
In 1988, Robinson
et al
.
5
reported a patient with WPW and
a coronary sinus anomaly, which was detected in necropsy. In
another report, in a series of 53 WPW patients, the incidence of
coronary sinus anomaly was found to be 13%.
6
Tebbenjohanns
et al
.
7
have conducted direct coronary sinus angiography in 43
patients with posteroseptal accessory pathways. They showed
that venous branch or coronary sinus anomalies were associ-
ated with the majority of patients with a posteroseptal accessory
pathway.
In our case, the patient had WPW syndrome. We attempted
ablation of the accessory pathway but were unsuccessful. He
later underwent electrode catheter ablation through a coronary
sinus branch.
The majority of free-wall accessory pathways are located in
the epicardial fat pad. Catheter ablation requires precise locali-
sation of the accessory pathway and delivers energy to that area
only. Occasionally but unusually, inferoseptal or left posterolat-
eral accessory pathways cannot be successfully ablated with the
use of an endocardial catheter, and energy needs to be delivered
within the coronary sinus or one of its branches. For left postero-
lateral accessory pathways that cannot be ablated from the endo-
cardium, a mid to distal coronary sinus location may be used.
8
The surface ECG may also provide some clues regarding
the location of the accessory pathway. The presence of a nega-
tive delta wave in lead II may correspond to the presence of an
inferoseptal accessory pathway located within the middle cardiac
venous system. Additionally, the presence of an initial R wave in
lead V1 may suggest the presence of a left inferoseptal accessory
pathway.
Attempts at accessory pathway ablation through the coronary
sinus using radio-frequency energy are associated with a success
rate in excess of 70%.
9,10
A major deterrent to accessory pathway
ablation within the coronary sinus or its branches may be the
greater potential for complications, compared with endocardial
ablation. Until recently, the most serious complications encoun-
tered were coronary sinus perforation with cardiac tamponade,
pericarditis and asymptomatic coronary sinus thrombosis.
10,11
Unfortunately, as this procedure has been performed quite
frequently, cases have been reported in which both clinically
significant and non-significant occlusions of the coronary arter-
ies (predominantly branches of the right coronary artery) adja-
cent to coronary venous branches have occurred.
11
It is therefore
very important that this procedure be performed with proper
surgical backup.
These anomalies alone are usually asymptomatic, although
they may complicate the mapping of the coronary sinus and
catheter ablation when associated with accessory pathways. As a
result, anomalies of the coronary sinus, as in this case, may be asso-
ciated with abnormalities of the conduction system of the heart.
Whether the combination of these types of anatomical anomalies
is a coincidence or whether there is an embryological link between
the accessory pathway and the coronary vein is not known.
Conclusion
Radio-frequency catheter ablation of an accessory pathway in the
coronary sinus can be effectively performed through the proxi-
mal portion of the middle cardiac vein. In view of more recent
reports of adverse sequelae, however, zealous performance of
such procedures should await the development and documenta-
tion of safer methodologies. In certain situations, referral for
surgical interruption of the accessory pathway may not be neces-
sary if the accessory pathway cannot be ablated from a more
conventional tricuspid or mitral annular location. In fact, in
the case described here, catheter ablation was successful where
previous ablations had failed.
Fig. 2. Coronary sinus aneurysm (arrow) on coronary
angiogram.