CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 5, September/October 2011
AFRICA
239
Discussion
Cardiovascular disease is the leading cause of mortality and
morbidity in adult patients in industrialised countries. The rela-
tionship between increased LDL-C levels and increased risk of
CHD is widely accepted, as is the corollary that lowering LDL-C
levels reduces CHD mortality. Hence, most practice guidelines
for CVD management focus on LDL-C as the primary target.
All guidelines encourage physicians to initially focus on
patients with established atherosclerotic disease as these stand
to gain the largest absolute short-term benefit, but preventive
measures in healthy individuals with a high global risk of CHD
(i.e. primary prevention) should also not be neglected.
16,17
The results of this survey indicate that most physicians are
aware of the current guidelines and that 95.0% of physicians
use them to set individual cholesterol targets for their patients.
Among all guidelines, the most frequently used was the National
South African guidelines (50.0%), followed by the NCEP ATP
III guidelines (35.9%) and the JETF guidelines (23.9%).
Despite the widespread awareness of recent guidelines, the
results of this survey indicate that the control of hypercholes-
terolaemia is sub-optimal. As highlighted by the EUROASPIRE
surveys
11,12
conducted in multiple European countries, the
CEPHEUS SA survey confirms that control of modifiable risk
factors remains sub-optimal in many patients at high cardiovas-
cular risk. For instance, obesity at 44.5% and smoking at 14.9%
remained highly prevalent. These results do not significantly
differ from those obtained in the two EUROASPIRE surveys,
18,19
and for certain modifiable factors, their current prevalence is
even higher.
The results of the current survey indicate that a large propor-
tion of patients on lipid-lowering pharmacological therapy in
South Africa failed to achieve their cholesterol goal levels. Only
60.5 and 52.3% of patients on LLD for at least the previous
three months attained the LDL-C target level recommended by
the 2004 updated NCEP ATP III guidelines and the lower target
proposed by the JETF/South African guidelines.
In agreement with the published literature, the percentage of
patients attaining the LDL-C goal was higher among patients
treated with statins. Statins have been shown to improve cardio-
vascular outcomes in a wide range of patients and are the most
powerful LDL-C-lowering drugs currently marketed.
20,21
The poor goal-achievement rates observed in the current
survey do not seem to be correlated with a poor awareness of
hypercholesterolaemia among patients. Most patients (73.3%)
were informed of their cholesterol level and had been given
a cholesterol target (80.4%). Most patients were aware of the
role of both LDL-C and HDL-C in CVD risk, and were satis-
fied with the level of information provided by their physicians.
Nonetheless, the level of knowledge of the general public
regarding dyslipidaemia seems to be much lower. In the REACT
survey,
22
physicians claimed that 92% of their patients knew
about LDL-C and HDL-C, but when members from the general
public were interviewed, only 23 and 25% of them were aware
of the importance of LDL-C and HDL-C, respectively. It is
assumed that in South Africa a large percentage of the population
do not know their cholesterol levels.
Although 60% of the patients have been reported to stop
taking their lipid-lowering medication once they reach their
cholesterol target in a prospective survey in Australia,
23
in this
survey which enrolled patients attending mainly for review
of lipid-lowering therapy, only 4% of the interviewed patients
acknowledged stopping their lipid-lowering therapy once they
had reached their goal.
Limitations
The present study has some limitations. Firstly, the population
was a selected group of patients treated with LLD, and the find-
ings cannot be extrapolated to the general population. More
motivated patients may have been more likely to agree to partici-
pation in the survey, introducing a potential positive bias. The
same bias could apply to the participating physicians. It is possi-
ble that not all patients completed the questionnaire truthfully,
but rather chose answers they thought would please their treating
doctor. CEPHEUS SA was performed as a survey, without inde-
pendent verification of the answers provided. The questionnaires
were not validated, but only used for exploratory purposes.
The diagnosis of metabolic syndrome was made using treated
lipid values. This may have resulted in some patients with the
metabolic syndrome being missed, as LLDs can lower triglycer-
ide and increase HDL-C levels. Untreated values for these lipid
variables were generally not available. Finally, caution is needed
when interpreting correlations, since causal relationships were
not established.
Conclusions
Overall, the results of this survey highlight the sub-optimal lipid
control achieved in many South African patients prescribed
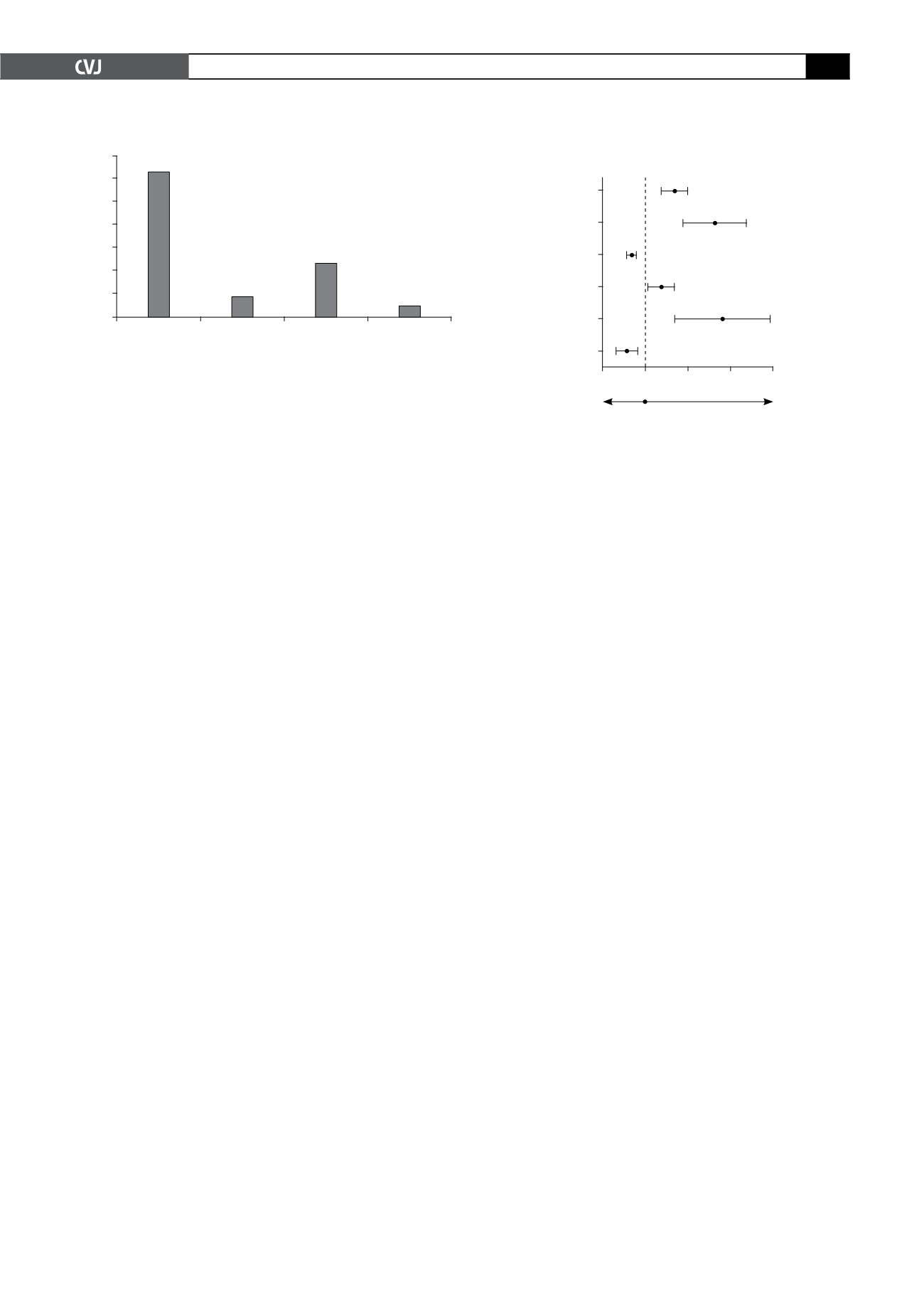
Fig. 3. Changes in LLD since first prescribed a drug.
70
60
50
40
30
20
10
0
Still on the
same tablet
Titrated up Changed
once or twice
Changed
several times
% of patients
63.5
8.7
23.2
4.6
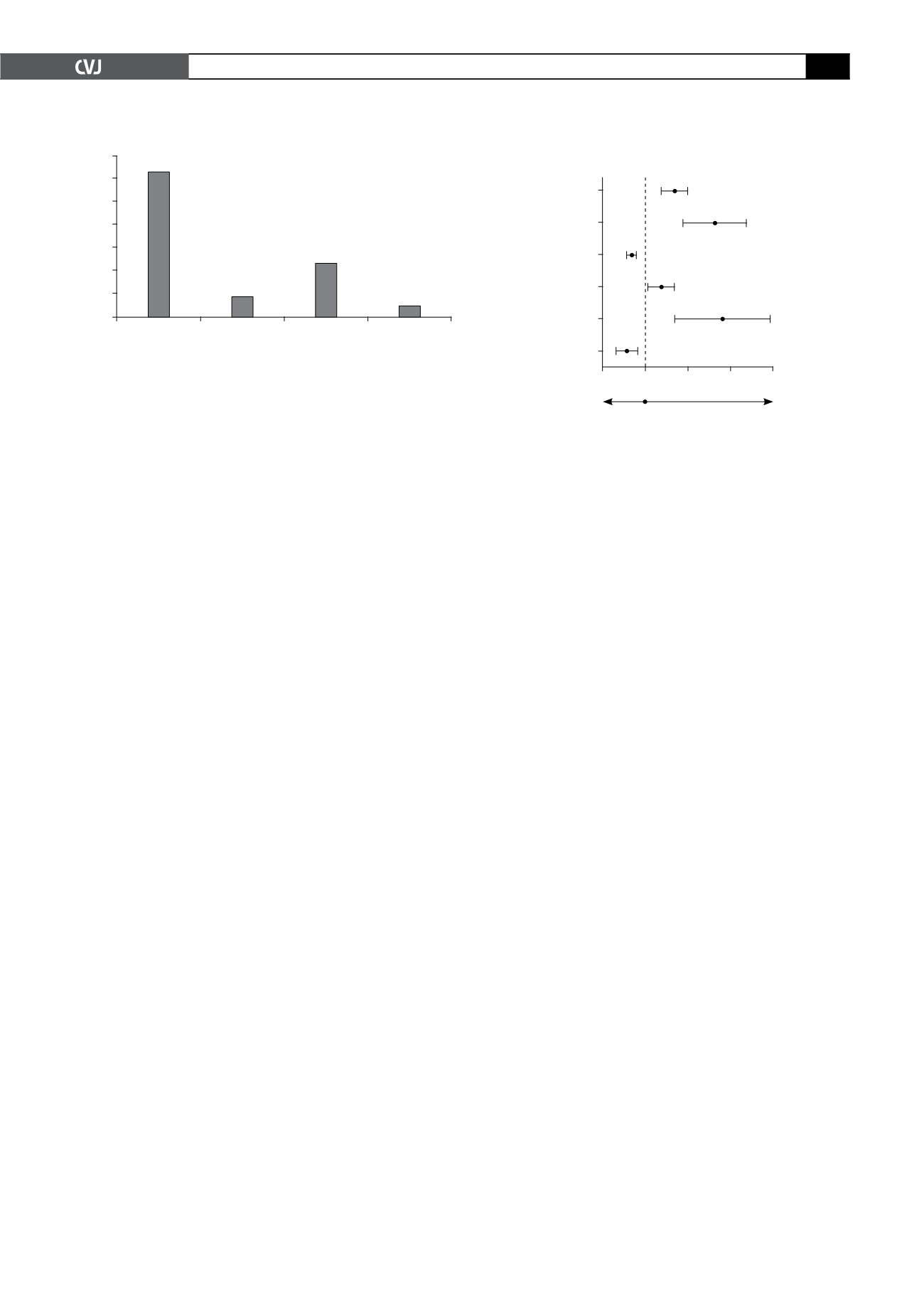
Fig. 4. Significant multivariate predictors of reaching the
NCEP LDL-C target levels.
Treatment
adherence
Medium/low risk vs
high risk
Female vs
male patient
Non-smoker
Age 55–70
vs
<
40
FH vs
primary prevention
1
2
3
4
[1.35; 1.97]
[1.86; 3.33]
[0.55; 0.78]
[1.05; 1.67]
[1.67; 3.90]
[0.30; 0.80]
95% CI
1.63
2.49
0.65
1.32
2.55
0.49
Odds ratio plot (multivariate analysis
Poor control
Good control