CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 5, September/October 2011
246
AFRICA
aorta before age 50 years.
Lumbosacral dural ectasia on computerised tomography or
magnetic resonance imaging is also a major finding. Other minor
findings are spontaneous pneumothorax and apical blebs in the
pulmonary system, striae atrophicae (stretch marks) that are not
related to marked weight gain, pregnancy or repetitive stress, and
recurrent or incisional hernia. The presence of a mutation that
causes MFS in FBN1, a first-degree relative who independently
meets the diagnostic criterion, and the presence of a haplotype
around FBN1 inherited by descent and unequivocally associated
with diagnosed MFS in the family are accepted as major findings
in the family history.
1-3
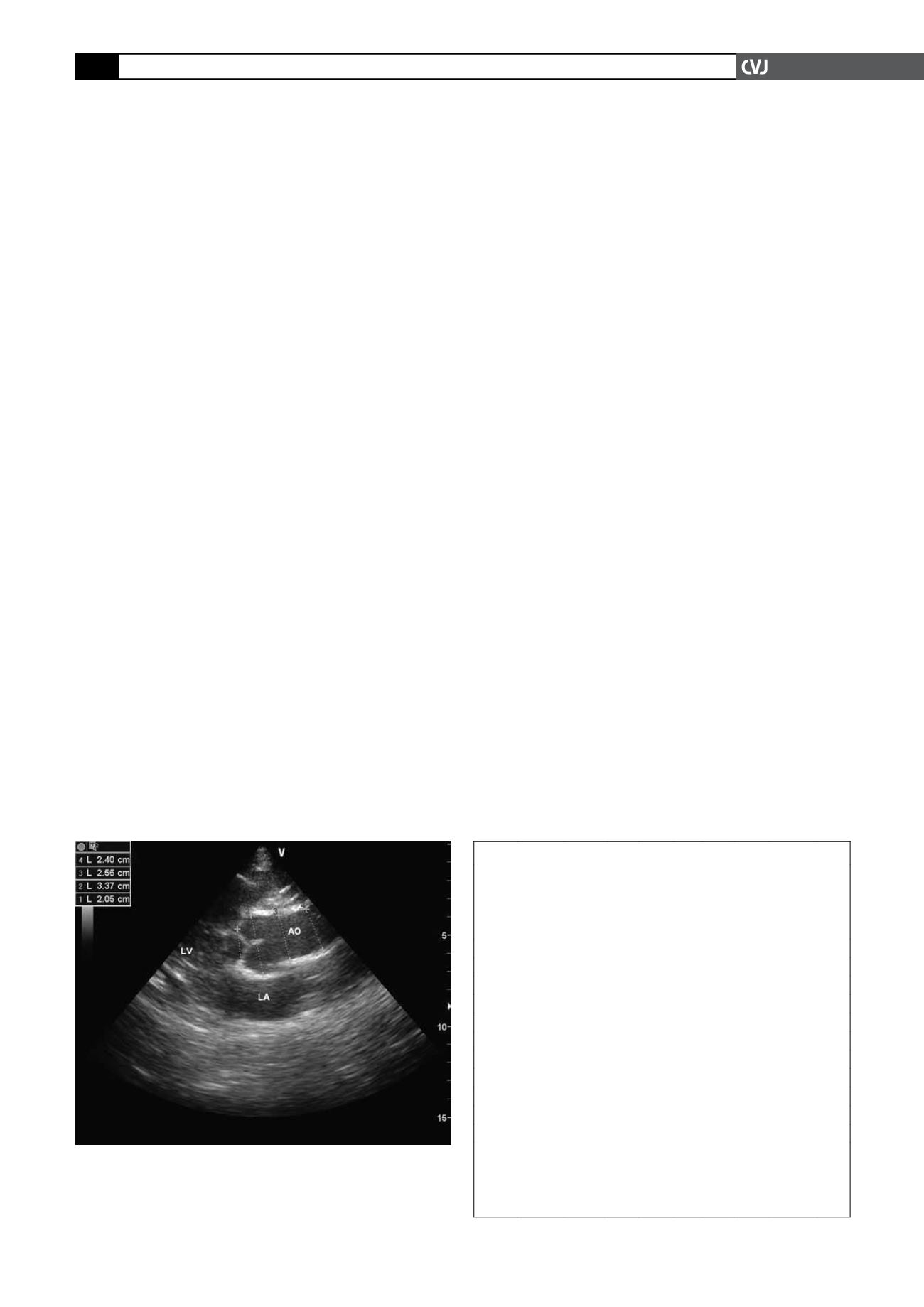
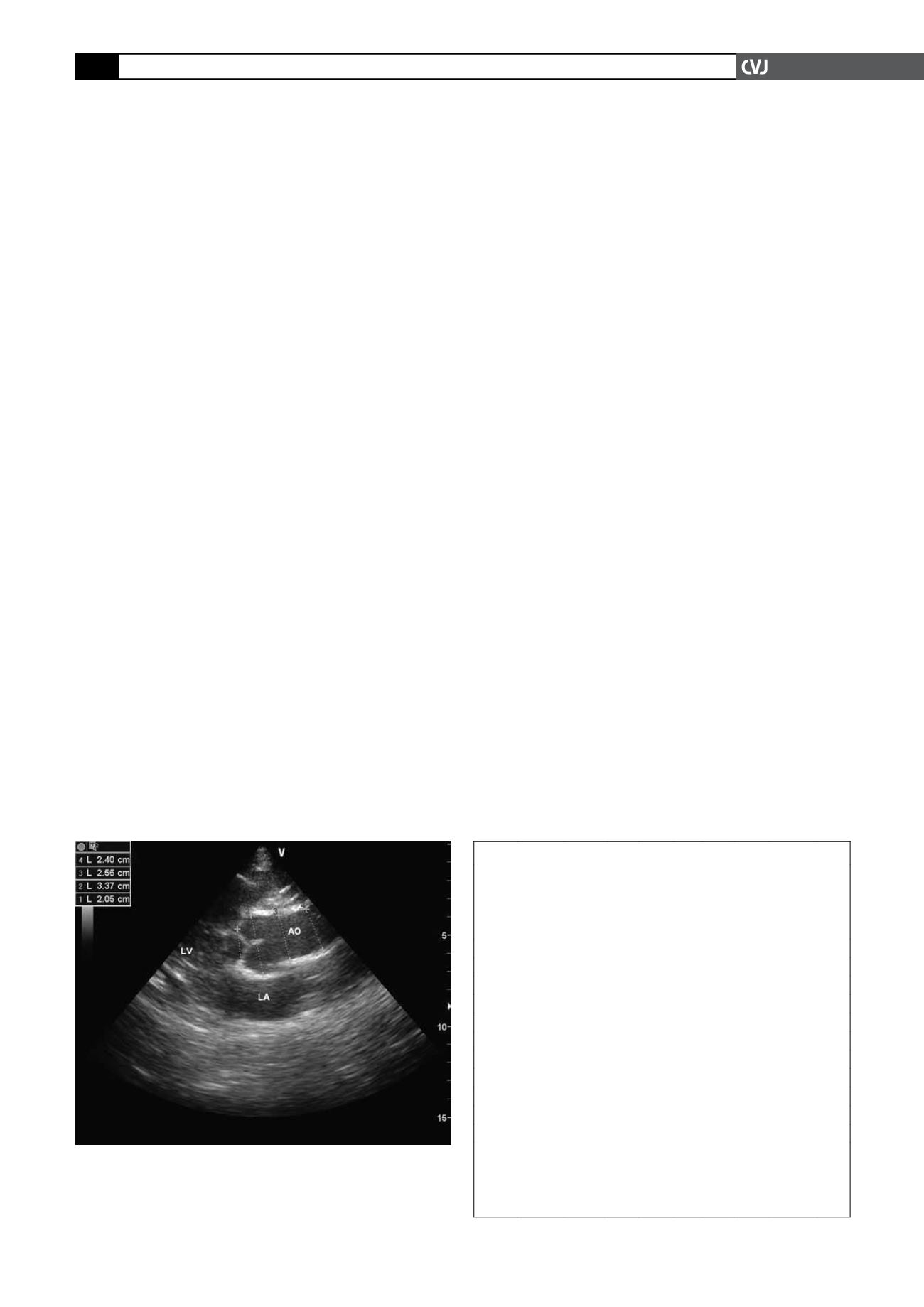
Using a commercially available echocardiographic system
(General Electric Vivid 3 with 7- and 3-MHz probes), mitral and
tricuspid valves were evaluated in particularly the parasternal
long-axis and apical four-chamber views. Mitral valve prolapse
and tricuspid valve prolapse (TVP) were defined as the presence
of leaflet thickness
>
5 mm and systolic prolapse of the leaflet(s)
into the atrium for more than 2 mm.
6
During colour and pulse-wave Doppler assessment,
>
1 cm
colour regurgitation jet, peak flow velocity of the regurgitation
flow
>
2.5 m/s, and regurgitation flow during the systole or late
systole were accepted as mitral regurgitation.
7
Aortic regurgita-
tion was defined as mosaic colour jet flow from the aortic valve
to the left ventricle during diastole. Aortic root dimensions were
measured at the level of the sinuses of Valsalva in M-mode and
cross-sectional views (Fig. 1). Diagnosis from dilatation of the
aortic root was based on the monogram described by Roman and
colleagues.
8
Results
Eleven patients (four female and seven male, age range 4–15
years, median 11 years) presentingMFS phenotyping characteris-
tics were diagnosed as MFS using the Ghent criteria.
3
All patients
had a physical examination and echocardiographic evaluation.
Clinical characteristics of the patients are reported in Table 1.
The most notable clinical feature at the time of presenta-
tion was height equal to or greater than the 97th percentile.
Arachnodactyly was found in all except one child. Nine patients
had arm span-to-height ratio
>
1.05. Eight subjects had a chest
deformity. A pectus carinatum deformity was documented in
five patients, while the excavatum deformity was noted in three
subjects. A scoliosis was present in seven patients. Seven chil-
dren had pes planus, which in most was associated with joint
hypermobility. Highly arched palate with crowding of teeth was
seen in 10 of 11 individuals. The classical facial features of MFS
were noted in nine children. Ectopia lentis was found in only
one subject. Three individuals had severe myopia (greater than 5
dioptres). A mutation in FBN1 was found in seven patients. No
child experienced striae atrophicae, lumbosacral dural ectasia or
spontaneous pneumothorax.
Regarding cardiovascular features of the patients, the ventric-
ular functions were within normal limits. Mitral valve prolapse
was documented in all patients, nine of whom had associ-
ated MR, whereas seven children had TVP. Eight patients had
prolapse of both mitral valve leaflets while three of the patients
with MVP had anterior leaflet prolapse. Dilatation of the aortic
root was found in six patients (patient no 2, 3, 4, 6, 7 and 10).
The range of the aortic root diameter was 16–43 mm and the
median was 24 mm. The widest aortic root diameter recorded
was 43 mm in a 15-year-old boy (10th case). None had an aortic
dissection while two had AR. In the study, the fourth case (four
years old and male) had all cardiac manifestations (MVP, MR,
TVP, dilatation of the aortic root, and AR).
Table 1 summarises the aortic root dimensions at the level of
the sinuses of Valsalva, and the other findings of echocardiogra-
phy. Figs 2 and 3 show examples of MVP, dilatation of the aortic
root, MR and AR.
Discussion
In MFS, cardiovascular disorders without appropriate treatment
are the main cause of mortality in the first four decades of life.
Extending survival depends on treatment or preventing compli-
cations of cardiovascular diseases such as dilatation of the aortic
TABLE 1. PATIENT CHARACTERISTICS
Patient
no
Gender
Age
(years)
BSA
(m
2
) MVP MR TVP
ARD
(mm)
Limits
of ARD
based
on BSA
(mm) DAR
1
F
5 0.68 PAL
+
– 16 14–21 –
2
F
7 0.97 PBL
+ +
28 17–24
+
3
M 14 1.61 PBL –
+
33 23–29
+
4
M 4 0.69 PAL
+ +
24 14–21
+
5
F
11 1.04 PBL
+ +
18 17–24 –
6
M 13 1.55 PBL
+ +
33 22–28
+
7
M 14 1.65 PBL
+ +
37 23–30
+
8
F
8 1.00 PBL
+ +
19 17–24 –
9
M 4 0.66 PBL
+
– 16 14–21 –
10
M 15 1.77 PBL
+
– 43 25–31
+
11
M 11 1.23 PAL – – 21 19–26 –
AR: aortic valve regurgitation; ARD: aortic root diameter; BSA: body
surface area; DAR: dilatation of the aortic root; F: female; M: male; MFS:
Marfan syndrome; MR: mitral regurgitation; MVP: mitral valve prolapse;
PAL: prolapse of anterior leaflet; PBL: prolapse of bileaflet; TVP: tricus-
pid valve prolapse;
+
: present; –: absent.
Fig. 1. Aortic root measurements with cross-sectional
echocardiographic examination. (1) annulus of the aorta,
(2) sinuses of Valsalva, (3) supra-aortic ridge, (4) proxi-
mal ascending aorta. AO: aorta, LA: left atrium, LV: left
ventricle.