CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 5, June 2012
AFRICA
283
compare echocardiographic differences between tuberculous and
idiopathic pericardial effusions.
20
The prevalence of ECP in these
two studies was 4.3 and 14.8%, respectively.
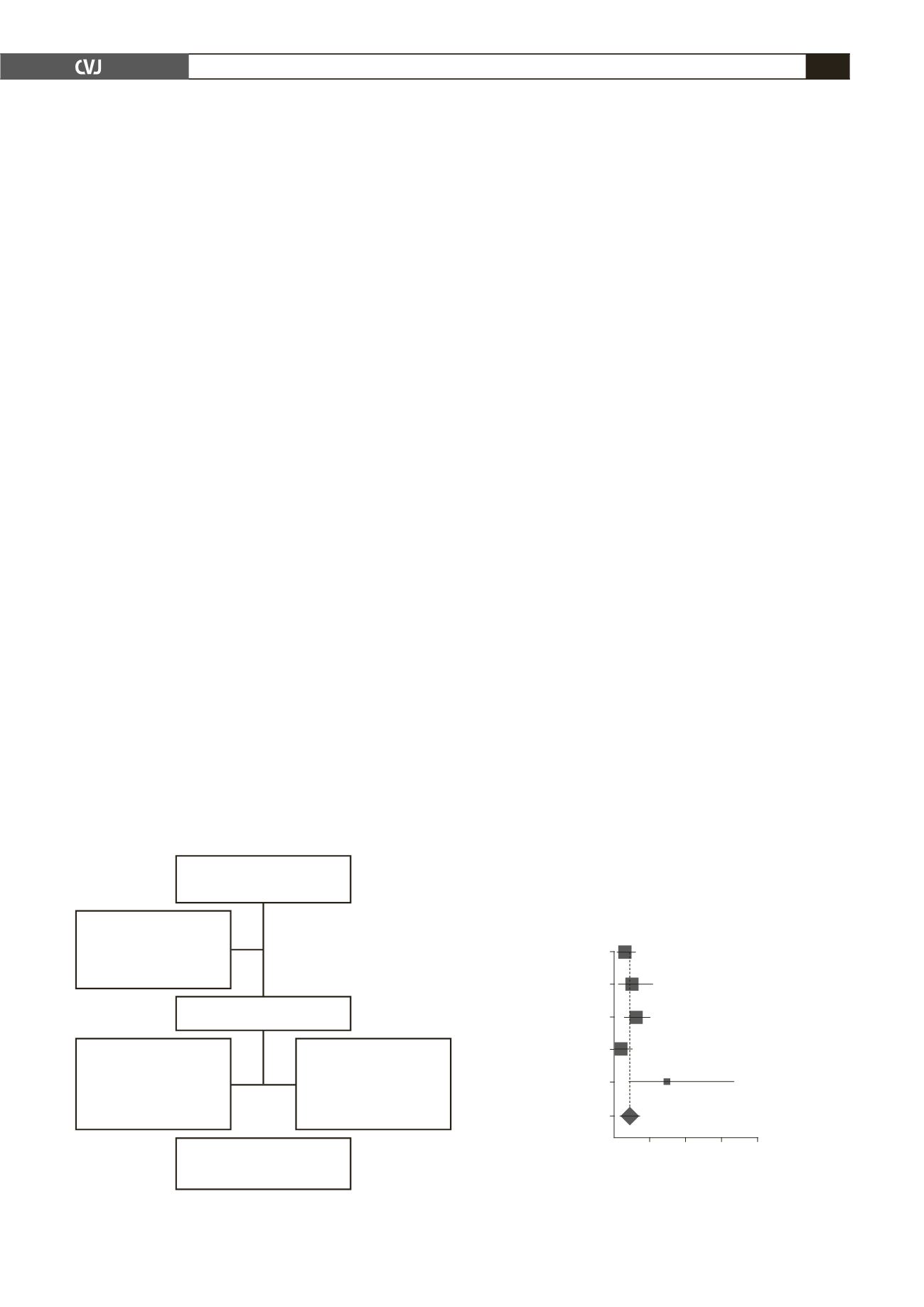
Overall there was significant variability in the prevalence
of ECP across the five studies (
p
= 0.04;
I
2
= 61%); therefore
we used both the random-effect and fixed-effect meta-analysis
models to combine the prevalence. Using the fixed-effect model,
the pooled prevalence of ECP in the five studies was 4.0% (95%
CI: 2.7–5.7%). This increased marginally to 4.5% (95% CI:
2.2–7.5%) using the random-effects model (Fig. 2).
Outcomes of patients with effusive constrictive
pericarditis
One-year mortality data was available for only nine participants
with non-malignant disease from two studies.
19,22
These mortality
rates are provided in Table 2.
Two of the nine patients were dead at 12 months; one from
peri-operative complications, and the other with tuberculous
ECP died while awaiting pericardiectomy. The combined death
rate across the studies was 22%, with wide 95% confidence
intervals (4–50%) due to the small numbers involved. Seven
patients did not undergo pericardiectomy. These seven included:
the patient with tuberculosis who died from heart failure while
awaiting surgery, three participants, also with tuberculosis,
who did not consent to the procedure, and three participants
with idiopathic disease in whom a conservative ‘wait-and-see’
approach had been adopted. The six participants, who survived
the early stages of their illness without surgery were alive and
well at their last follow-up visit.
Only three of the studies provided data on the pericardiectomy
rates.
3,19,22
Overall, the combined pericardiectomy rate was
65% (95% CI: 43–82%) and the between-study variability in
pericardiectomy rates was marginally significant (
p
= 0.10;
I
2
=
56%). A breakdown of the pericardiectomy rates by aetiology
revealed that 73% of participants with idiopathic ECP, 60% of
those with tuberculous ECP, and 50% of those with ECP of other
aetiologies underwent the pericardiectomy.
The persistence of heart failure was the reason for surgery in
54% of cases, making it the most common indication, followed
by prophylaxis against progression to fibrous constrictive
pericarditis in 23%. Recurrence of pericardial effusion was an
indication in 15%. In only 8% was the operation performed
studies were included in the systematic review.
3,19-22
The five
studies had a total of 642 patients, 26 of whom met diagnostic
criteria for ECP; 58% (15/26) had probable ECP and 42%
(11/26) definite ECP. Of the 26 patients, 50% (13/26) had
idiopathic pericarditis, 38% (10/26) had tuberculous pericarditis,
8% (2/26) had post-radiation pericarditis and 4% (1/26) post-
pericardiotomy pericarditis.
Prevalence of effusive constrictive pericarditis
The study design and strength of diagnosis of ECP varied
across the five selected studies. Three of the five studies were
prospective cohorts.
3,19,21
One of the three prospective case
series was a single-centre South African study, designed to
determine the 30-day and one-year outcomes of consecutive
patients with predominantly tuberculous pericarditis, who were
each given a standardised therapeutic protocol, which included
pericardiocentesis.
19
The proportion of those with ECP was 2.6%
based on clinical and echocardiographic criteria.
The second prospective case series was a single-centre
French study designed to determine the role of surgical
pericardioscopy as a diagnostic tool among patients with large
pericardial effusion of uncertain aetiology.
21
The proportion of
patients diagnosed with ECP was reported as 1.4%. All patients
underwent pericardiocentesis, and echocardiography was used to
assess pericardial physiology and content.
The third prospective case series was a single-centre Spanish
study, which aimed to determine the prevalence of ECP and the
incidence of pericarditis-related outcomes over a median follow-
up period of seven years.
3
Consecutive participants presenting
with a diagnosis of pericardial tamponade over 15 years
underwent measurement of the pre- and post-pericardiocentesis
intra-pericardial and right atrial pressures. The prevalence of
ECP was 5.8% in those patients undergoing pericardiocentesis,
6.8% in those with clinical tamponade, and 0.93% in patients
with any pericardial disease.
3
The remaining two studies of patients with a probable
diagnosis of ECP were designed to (1) determine the long-
term outcome of patients with symptomatic effusion;
22
and (2)
Fig. 2. Forest plot for the prevalence of ECP (random
effects).
Reuter 2007
Tsong 2003
Sagrista-Sauleda 2004
Nugue 1995
George 2004
Combined
0 10 20 30 40
Prevalence (95% confidence interval)
2.5% (0.9, 6.0)
4.3% (1.2, 10.8)
5.5% (2.9, 10.1)
1.4% (0.2, 5.0)
14.8% (4.2, 33.7)
4.5% (2.2, 7.5)
Fig. 1. Flow chart for selection process.
1 138 potentially relevant
publications
1 089 articles
eliminated after
review of the titles
and abstract
49 articles evaluated
Three studies
excluded because
diagnosis of ECP
established by clinical
assessment only
No data on proportion
of patients with ECP
in 41 studies
Five articles selected for
inclusion in review