CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 5, June 2012
278
AFRICA
Complications
Eighty-six patients (91%) completed the postoperative
in-hospital period and were discharged without any remarkable
complication. There were four minor complications. One patient
had a groin haematoma and one had meralgia paresthetica, both
of which resolved spontaneously and were most likely related to
the large 14F sheath used for Artisan™. One patient developed
congestive heart failure 24 hours post procedure, which was
related to the underlying structural heart disease and significant
fluid infusion (at 17 ml/min) necessary at the time for cooling
of the ablation catheter. Septicaemia was suspected in one case,
which was probably co-incidental and was controlled with
antibiotic therapy and supportive measures.
There were two intermediate-level complications. One patient
developed a groin arteriovenous fistula, which was related to the
large 14F sheath and was repaired surgically. One patient had late-
onset pericardial effusion (on postoperative day 10), which was
most likely related to fluid overload and inflammatory response
to ablation and was treated successfully with pericardiocentesis.
There were three major complications. One patient had
cardiac tamponade, treated immediately with pericardiocentesis.
The patient was female and rather small in size. Another patient
had left atrial perforation, which was repaired surgically.
Similarly, the patient was female and rather small in size. This
case was caused by ‘catheter snap’ during ablation on the upper
aspect of the ridge between the appendage and left superior
pulmonary vein (LSPV). Poor tissue quality/elasticity probably
contributed to this complication, as the patient had rheumatoid
arthritis and was on long-term methotrexate therapy.
One patient had aspiration pneumonia and blurring in the
right eye due to embolus; his vision recovered after two months.
This complication occurred because the patient was morbidly
obese (160 kg) and it was difficult to keep his ACT above
250 s; he seemed resistant to unfractionated heparin. No case
of pulmonary vein stenosis, transient ischaemic attack or stroke
was reported throughout the post-procedure follow up.
Follow up for relapse
As of March 2011, patients were followed up for an average of
13.4
±
3.6 months. A freedom from AF of 94.7% was achieved
after an average of 1.15 attempts per patient. One patient
refused to undergo more attempts after developing relapse,
and four patients (4.2%) finally underwent AV node ablation
with placement of a permanent pacemaker, one of which had
developed late-onset relapse 13 months after robotically assisted
ablation. Five patients (5.3%) underwent a redo ablation within
the six-month follow up, seven patients (7.4%) had a redo
procedure after six months, and one patient received two redo
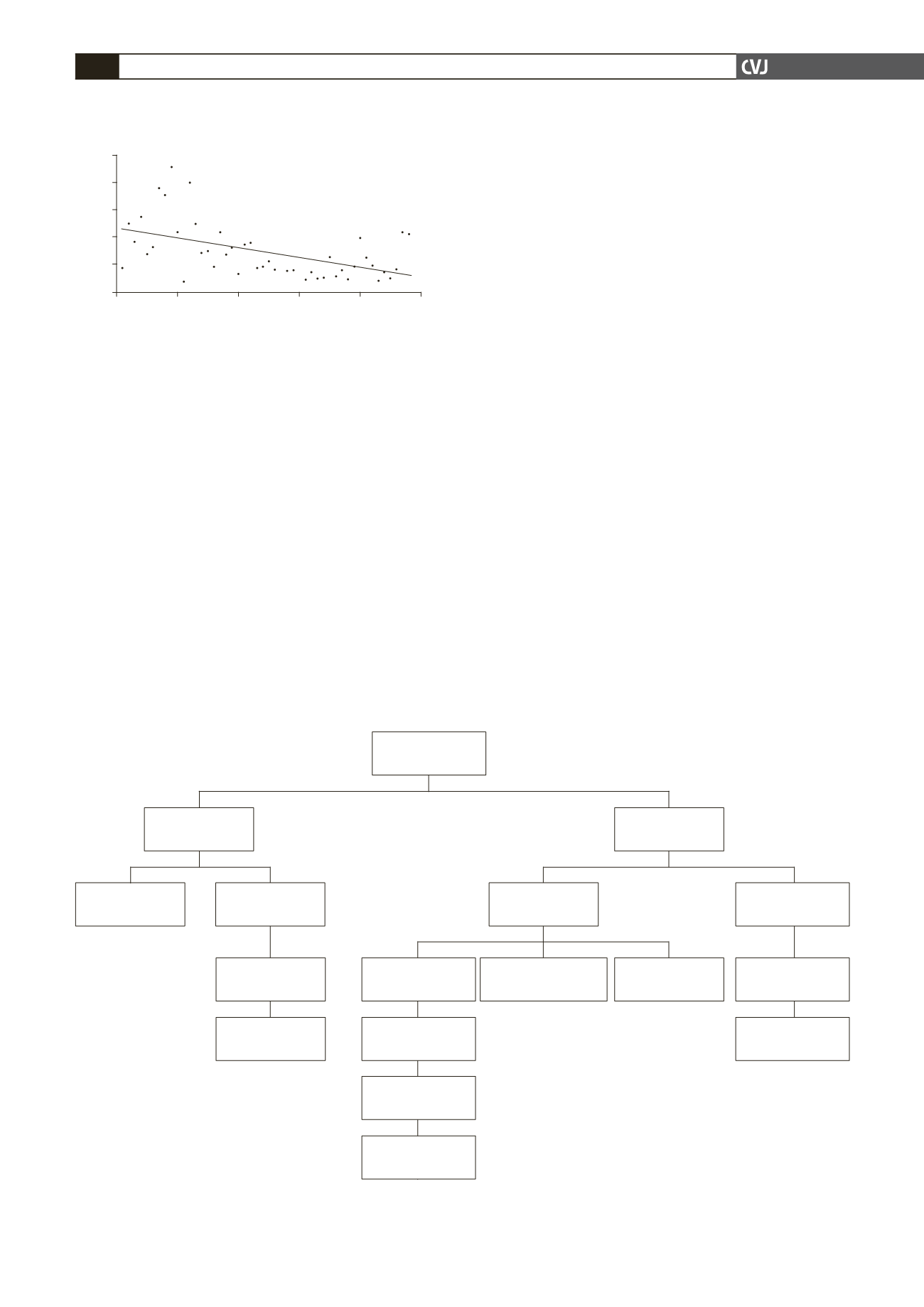
Fig. 2. Scatter plot showing a decrescendo trend in
screening time for the first half of the study group.
100
80
60
40
20
0
Screening time (min)
0
10
20
30
40
50
Patient number
y
=
–0.7012
x
+
46.979
R
2
=
0.2488
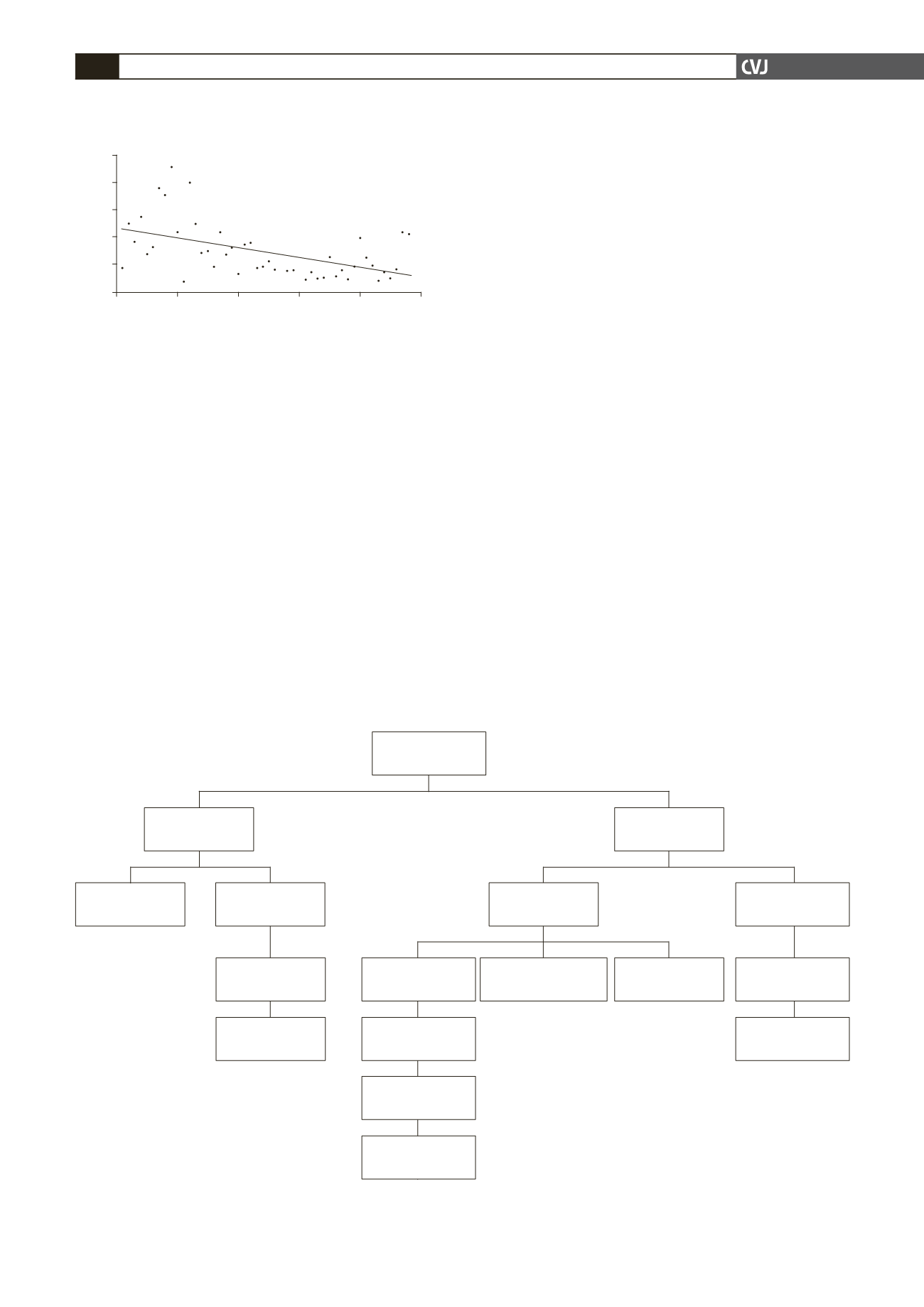
Fig. 3. Flow chart showing outcomes for the whole study group; AAD, antiarrhythmic drugs; AVN, atrioventricular
node; PPM, permanent pacemaker.
17 developed
relapse
78 free from
relapse
69 off AAD
1 AVN ablation
(already had a PPM)
2 without redo
ablation
95 patients
1st robotic ablation
6 on previously
ineffective AAD
3 on new AAD
9 on AAD
2 relapse after
6 months
1 without redo
ablation
1 AVN ablation +
PPM after 1st redo
15 relapse within
6 months
12 redo ablation
1 controlled after
2nd redo
2 AVN ablation +
PPM after 1st redo
9 controlled after
1st redo