CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 5, June 2012
AFRICA
279
ablations at five and 10 months (Fig. 3).
The nine-month follow-up period was completed for 100%
of patients; no cardiac mortality was observed among the study
population within the nine-month period. However, one patient
died of prostate cancer seven months post ablation. After one
attempt, 26 patients (27.4%) were discharged from hospital off
any sort of AADs.
At nine months’ follow up, 70 patients (73.7%) were free
from arrhythmia off AADs, and 10 (10.5%) were AF-free on
AADs, yielding a total freedom from AF of 84.2% without
any redo procedures (Table 3). Considering those patients who
relieved completely after a redo procedure within the nine
months post ablation, freedom from relapse rose to 88.4%.
Multivariate logistic regression analysis showed that longer-
standing types of AF and ablation (radiofrequency) time are
independent predictors of arrhythmia relapse within the nine-
month period post ablation therapy (Table 4).
Discussion
This is the first report on mid-term efficacy of robotically
navigated catheter ablation in an unselected subset of patients
with predominantly persistent AF. Overall success rate without
any redos reported in this study is comparable to the results
obtained in the largest randomised, controlled trial (
n
=
390
total; 197 robotic arm) performed to date by Di Biase
et al.
(84.2
v 85%).
11
In the subset of patients with persistent AF, the results
of this study compare favourably to that reported by Di Biase
et
al
. (82 vs 70.9%).
11
These results bolster our confidence in the
robotic system as an efficacious treatment modality for patients
with persistent AF.
The overall mid-term success rate of 88.4% after the 1.12
procedures per patient reported in this study is comparable to the
results reported by Hlivak
et al
. (
n
=
69, success rate 86% after
1.2 procedures per patient).
13
These studies consistently show
that robotic ablation is also a clinically viable option for redo
procedures in patients who do not respond to ablation on the
first attempt.
Recently, an updated worldwide survey on the methods,
efficacy and safety of manual catheter ablation for AF showed
that across all surveyed centres, median overall success rates were
84.0% (79.7–88.6%;
n
=
9 590), 74.8% (66.1–80.0%;
n
=
4 712)
and 71.0 (67.4–76.3%;
n
=
1 853) for paroxysmal, persistent and
long-standing AF, respectively. For the main subset of patients
in this study (i.e. patients with persistent AF), we see that overall
success rate with the robotic ablation compared favourably with
that of manual ablation. Given that robotic ablation technology,
techniques and catheters are still in their infancy, the efficacy of
this treatment modality has the potential to reliably surpass its
manual counterpart in the near future.
As shown by the multivariate analysis, longer-standing
types of AF and ablation (radiofrequency) time are independent
predictors of arrhythmia relapse within the nine-month period
post ablation therapy (Table 3). As described in the methods
section, some of the more complex cases required ablation along
the endocardial aspect of the coronary sinus or in an attempt to
terminate the flutter or focal atrial tachycardia in addition to the
standard PV isolation. Therefore, longer ablation time in fact
points to a more complex underlying arrhythmia circuitry, which
is the most likely explanation for its correlation with higher
frequency of relapse. Association of long-standing AF type with
higher relapse rate may also be related to the same aetiology.
In general, because the robotic navigation system significantly
reduces physical operator strain, mitigates concerns over
excessive radiation exposure during complex cases, and enables
operators to perform complex ablation patterns regardless
of catheter skills, operators are more likely to take on more
complex and challenging AF cases. Hence, we expect to see
longer ablation times as a surrogate for more complex cases
associated with higher relapse rates in future studies.
As shown in Fig. 1, mean procedure and fluoroscopy times
were statistically reduced after the first fifth of the patients (
n
=
19). Furthermore, fluoroscopy time showed a linear decrescendo
trend for the first half of the patients (
n
=
48), after which point
it reached a plateau. This observation was in line with the results
reported by Di Biase
et al
., who showed statistically significant
reduction in fluoroscopy time after the first 50 cases.
11
These
observations confirm that there is a learning curve in using
the robotic navigation system and that operators can anticipate
further reduction in fluoroscopy time, and hence safer operation
once they overcome this learning curve. Reduction in procedure
time allows for shorter cases, less physical operator strain and
higher laboratory throughput.
Regarding major complications related to the robotic
navigation system, specifically the incidence of cardiac
tamponade and left atrial perforation, Hansen Medical’s new
Lynx™ catheter, which is smaller in size (requires a 12F sheath)
and more gentle (less rigid and lighter) than the Artisan™
catheter used in all the procedures reported herein, will probably
reduce the risk of these complications, especially in small
female patients with previous tissue quality/elasticity problems.
Arteriovenous fistula, considered here as an intermediate-level
complication, will likely occur less frequently with the new
Lynx™ catheter that requires a 12F sheath as opposed to the 14F
sheath size of Artisan™.
Additionally, the next generation of ablation catheters such
as Carto SF (Biosense-Webster, Diamond Bar, CA, USA),
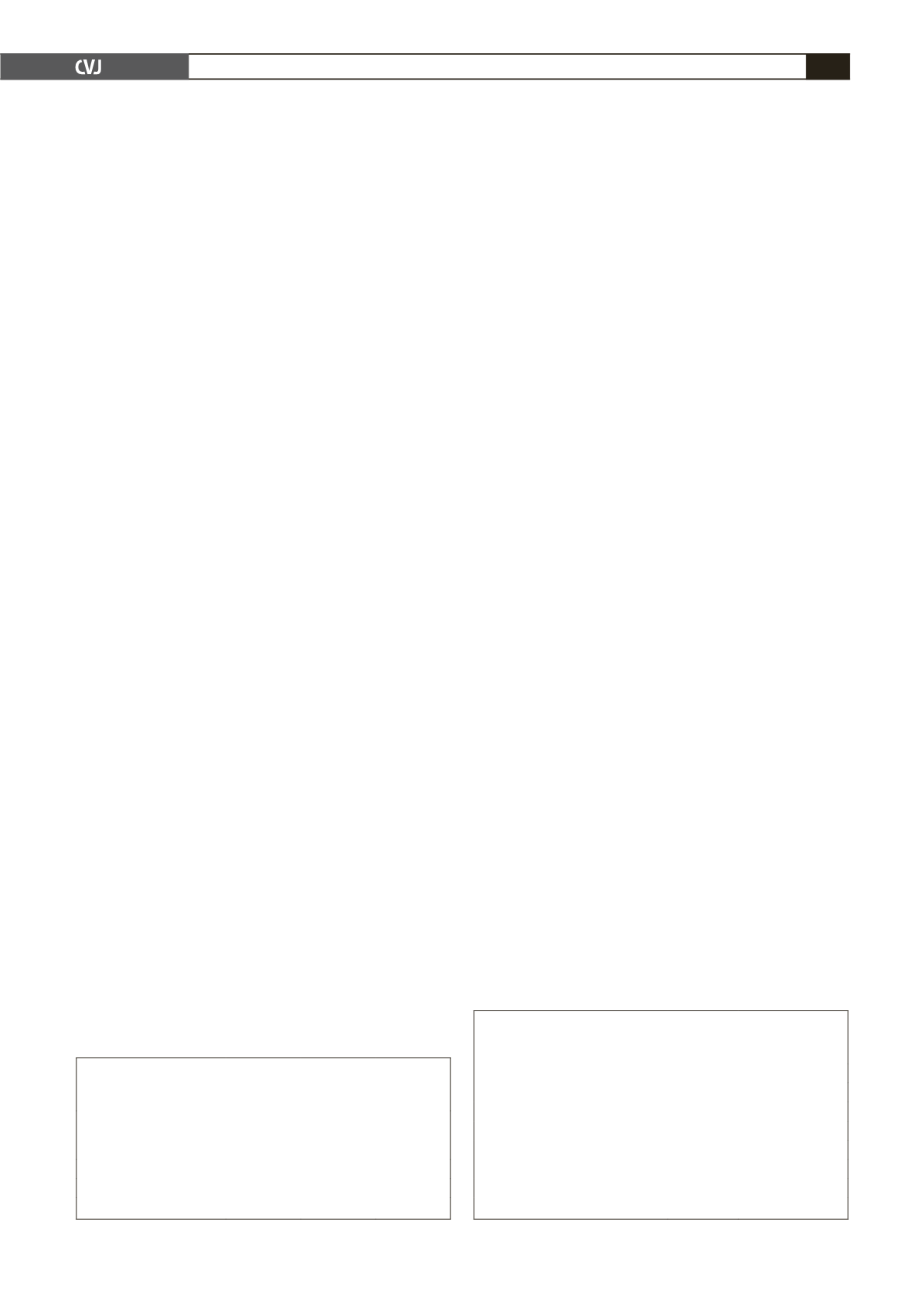
TABLE 3. FIRST-ATTEMPT SUCCESS RATES
IN RELATION TOTHE TYPE OFAFAND
ANTIARRHYTHMIC DRUGS (AADs)
Type of AF
Success off
AADs
n
(%)
Success on
AADs
n
(%)
Overall
success
n
(%)
Paroxysmal
12/12 (100) 1/1 (100) 13/13 (100)
Persistent
57/58 (98)
6/19 (32)
63/77 (82)
Long-standing persistent
0/0
2/5 (40)
2/5 (40)
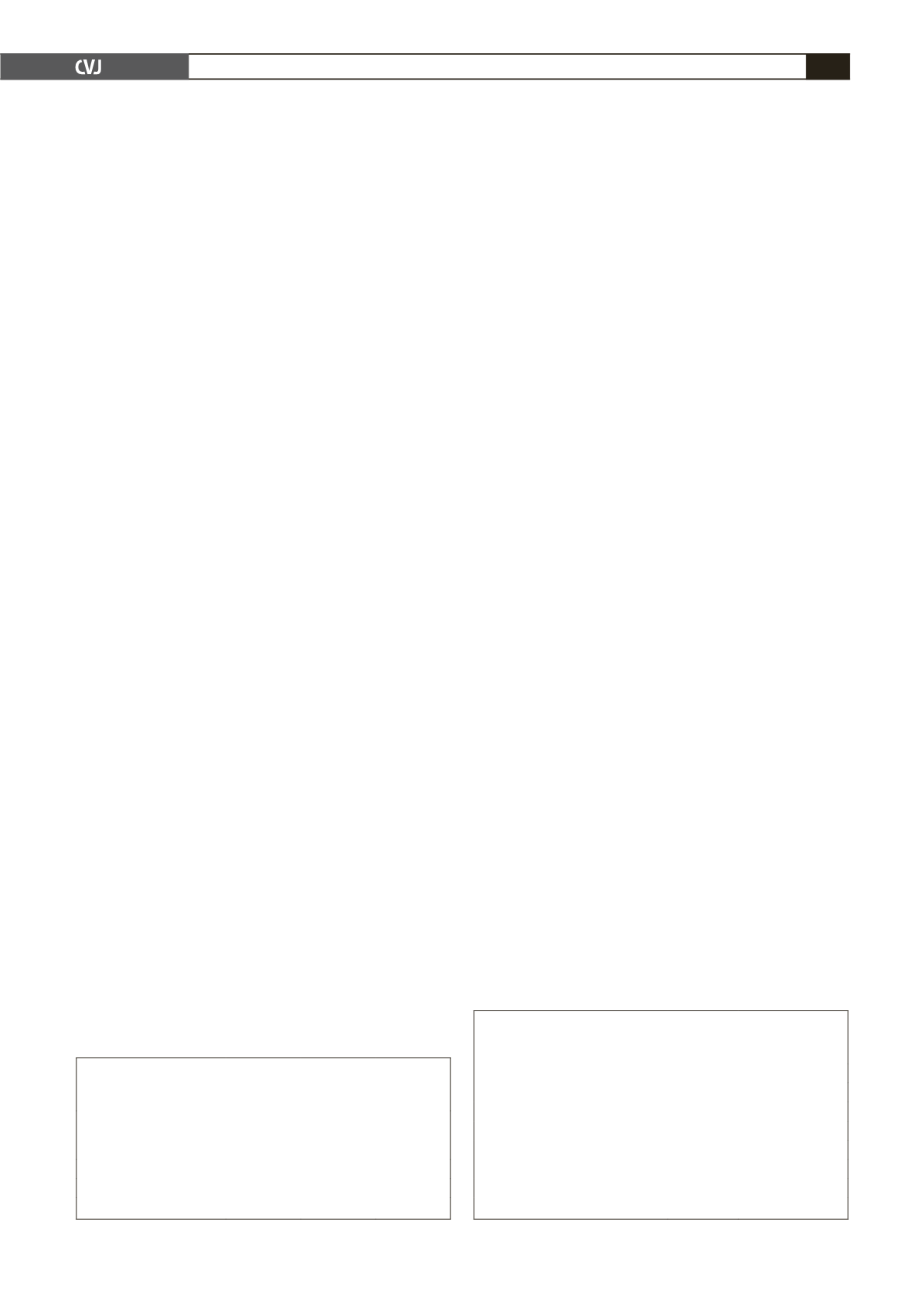
TABLE 4. MULTIVARIATE LOGISTIC REGRESSION
ANALYSIS OFAF RELAPSE PREDICTORS
AFTER ROBOTICABLATION
Variable
Odds Ratio
95% CI
Age
0.9957 0.9386–1.0562
Concomitant flutter
0.8580 0.2334–3.1539
AF type
12.8330 1.4454–113.9412
Mapping system/ablation catheter
1.8701 0.4034–8.6688
Procedure time
0.9835 0.9700–0.9973
Radiofrequency time
1.0508 1.0104–1.0929
Screening time
1.0177 0.9838–1.0527