CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 2, March 2013
AFRICA
25
The SOMANZ (Society of Obstetric Medicine of Australia
and New Zealand) classification and definitions of hypertensive
disorders of pregnancy were used.
12
However, for this research
purpose, the diagnosis of pre-eclampsia was based only on
hypertension and proteinuria from 20 weeks of gestation.
Proteinuria was considered as urine dipstick protein of 1+ or
more (on two occasions at least) or a 24-hour urine protein of
at least 300 mg. In addition, only women whose high blood
pressure had returned to normal values within a week of delivery
were included in the study to rule out chronic hypertension.
All women are offered counselling and voluntary testing for
HIV at these hospital sites as the standard of care. Institutional
ethical and hospital regulatory permission was obtained for the
study (Biomedical Research Ethics Committee, University of
KwaZulu-Natal, South Africa; reference number BE 151/010).
In the province of KwaZulu-Natal, the HIV/AIDS infection
rate in pregnant women is 40%.
10
Assuming a reduction in HIV
rate from 40% in controls to 25% in cases (pre-eclamptics), 890
women (445 cases and 445 controls) were required to achieve a
study power of 80% with statistical significance of
p
<
0.05. This
sample size was also estimated by assuming that the proportion
of HIV-infected women with a CD
4
cell count
<
200 cells/
µ
l
(immune-compromised) would be lower among pre-eclamptics.
Statistical analysis
SPSS version 18 was used to analyse the data. A
p
-value
<
0.05
was considered statistically significant. Pearson’s Chi-square
tests were used to compare categorical variables between cases
and controls, while
t
-tests were used to compare quantitative
variables between the two groups if the data were normally
distributed. Mann–Whitney tests were used if the data were
skewed. Binary logistic regression analysis was conducted in
order to assess the adjusted odds ratio for HIV status according
to the age and parity difference between the groups.
Results
There was a total of 23 988 deliveries over the study period at the
two study sites. Among them, 1 892 women were identified with
a diagnosis of pre-eclampsia (including imminent eclampsia, and
eclampsia).
Data were collected from 500 cases (pre-eclamptics) and
500 controls (normotensive healthy pregnant women) who met
the inclusion criteria. Among the pre-eclamptics, eight cases
had information missing from their files (birth weight and/or
gestational age at delivery) and were therefore excluded. Finally,
492 cases were used for analysis. The maternal age of the two
groups are shown in Table 1.
The rate of HIV infection in the pre-eclamptic group was
26.4%. In the control group, the HIV infection rate was 36.6%
(OR
=
0.62, 95% CI: 0.47–0.82,
p
=
0.001) (Table 2).
Pre-eclamptic women were 38% less likely to be HIV
infected than the control group without pre-eclampsia. Because
the cases and controls were not exactly age and parity matched,
the difference between them in HIV infection rate was adjusted
for this confounding factors using logistic regression analysis.
The odds ratio of being a case (pre-eclamptic) compared to a
control was 0.658 for HIV negative (
p
=
0.005) after adjustment.
This means that HIV-infected women were 34.2% less likely to
develop pre-eclampsia than women not infected with HIV.
The results of the CD
4
counts were available in only 66 cases
(pre-eclamptics) and 75 controls.
In women with pre-eclampsia, the median CD
4
count was 304
cells/
µ
l with a maximum of 906 cells/
µ
l and a minimum of 10
cells/
µ
l, versus 208 cells/
µ
l with a maximum of 725 cells/
µ
l and
a minimum of 56 cells/
µ
l in the control group (
p
=
0.008). The
proportion of pre-eclamptic women with
≥
3+ protein was higher
in the HIV-negative group (39.2%) than in the HIV-positive
group (27.9%) (
p
=
0.022).
Discussion
As far as we know, this is the first study to report the rate of HIV
infection in women with pre-eclampsia in comparison with a
control group without pre-eclampsia. Most studies on HIV and
pre-eclampsia have compared the rate of pre-eclampsia between
uninfected and HIV-infected women.
4,7-9
The rate of HIV/AIDS infection was lower in pre-eclamptic
women than in the control group. These findings suggest that
women with pre-eclampsia are less likely to be affected by
HIV infection than the general population. In other words,
HIV infection being the exposure and pre-eclampsia being the
outcome variable, HIV-infected women are at a lower risk of
developing pre-eclampsia. Our findings also suggest that HIV
infection could have a protective effect against the development
of pre-eclampsia.
The underlying mechanism of the protective effect of HIV
infection is unclear. As postulated in our hypothesis, it is possibly
associated with immune suppression in HIV-infected women.
To further evaluate this association, the level of immunity
(as expressed by the CD
4
count) between the two groups was
compared. The CD
4
count result, however, was available in only
66 cases and 75 controls. The median CD
4
count was lower in the
control group without pre-eclampsia (median CD
4
count
=
208
cells/
µ
l) than in the pre-eclamptic women (median CD
4
count
=
304 cells/
µ
l) (
p
=
0.008). This suggests that among HIV-infected
women, the immunity was less affected in those who developed
pre-eclampsia.
We also found that the proportion of pre-eclamptic women
with +3 protein or more in their urine dipstick was higher in
TABLE 2. HIV RATE IN CASESAND CONTROL GROUP
HIV positive
n
(%)
HIV negative
n
(%)
Total
n
(%)
Control group
183 (36.6)*
317 (63.4)
500 (100)
Pre-eclamptic group 130 (26.4)*
362 (73.6)
492 (100)
Total
313 (31.6)
679 (68.4)
992 (100)
*
p
=
0.001; OR
=
0.62; 95% CI: 0.47–0.82.
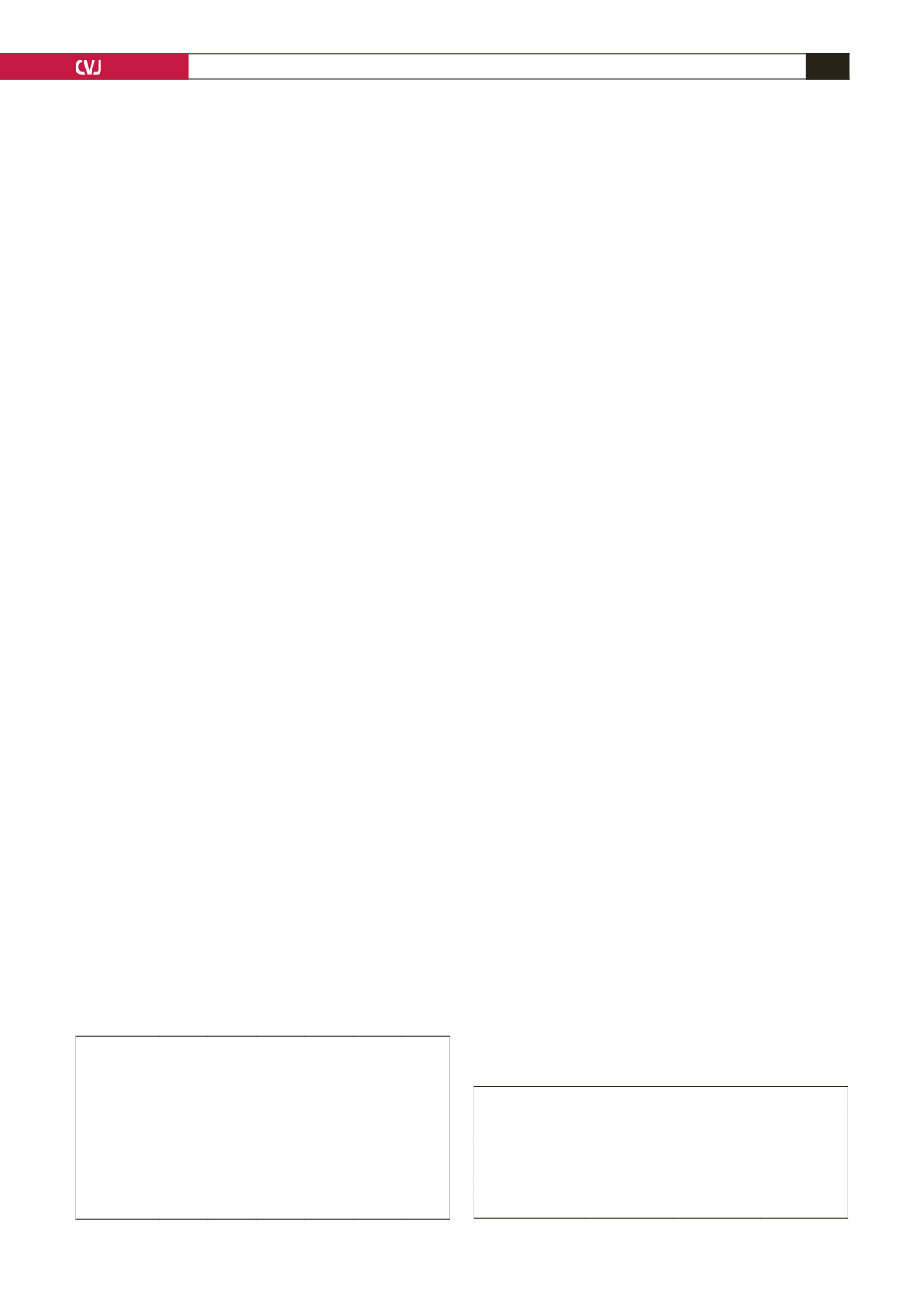
TABLE 1. MATERNALAGE DISTRIBUTION
IN CASESAND CONTROL GROUP
Age
< 20
years,
n
(%)
20–29
years,
n
(%)
30–39
years,
n
(%)
≥
40
years,
n
(%)
Mean
age
(years)
Total,
n
(%)
Controls
147
(29.4)
210
(42.0)
116
(23.2)
27
(5.4)
25.25 500
(100%)
Pre-eclamptics 145
(20.4)
250
(50.6)
93
(18.8)
6
(1.2)
24.09 492
(100%)
Total
292
(29.4)
460
(46.3)
209
(21.9)
33
(3.3)
24.67 992
(100%)



















