CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
334
AFRICA
distribution of lipid abnormalities for the entire sample and
then for sub-samples of very high-risk and non-very high-risk
patients. Additionally, joint distributions that either include or
exclude patients with no lipid abnormalities are provided for
each patient group.
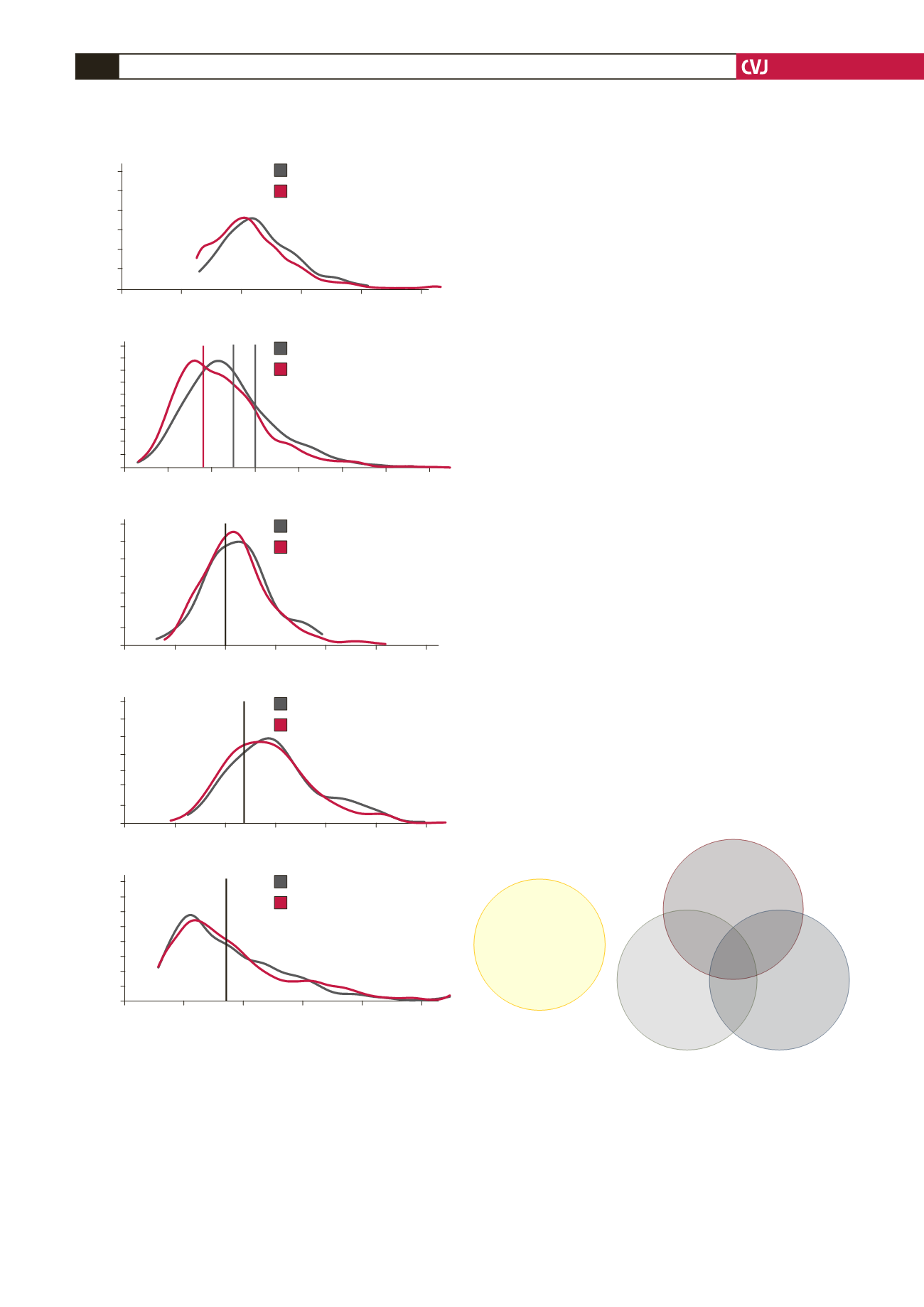
Fig. 3 shows that in 39.4% of patients with a total lipid
profile, there was only one single-lipid abnormality, 32.8% had
two abnormalities, and the remaining 7.3% had abnormalities
in all three assessed components of the lipid profile. Among
statin-treated patients, the most common abnormality was high
LDL-C levels (18.8% of all cases), accounting for 47.7% of all
single-lipid abnormalities. Among the 983 patients, 20.4% had
no lipid abnormalities.
Figs 4 and 5 present the joint distribution for non-very
high-risk and very high-risk patients, respectively, and indicate
different patterns of prevalence for these sub-groups. For the
261 non-very high-risk patients with at least one abnormality
depicted in Fig. 4, 37.2% had only one lipid abnormality, 21.5%
had two lipid abnormalities and the remaining 4.2% had all three
lipid abnormalities.
By contrast, for the 826 very high-risk patients depicted in
Fig. 5, the majority, 45.4%, had two or more lipid abnormalities
(40.2% had one, 37.0% had two, and the remaining 8.4% had
all three). For non-very high-risk patients, elevated triglycerides
were the largest single abnormality present, appearing in 42.2%
of all non-very high-risk patients. By contrast, among very
high-risk patients, high LDL-C level was the most frequent
abnormality, at 60.1% of all very high-risk patients.
Variables independently associated with
dyslipidaemia
Multivariate logistic regression analyses indicated that among
the 19 risk factors incorporated into the model, mixed ancestry,
along with history of hypertension, DM and cerebrovascular
disease were among the risk factors strongly, positively and
No lipid abnormalities
20.4%
(201)
18.8%
(185)
8.6%
(85)
8.9%
(87)
15.7%
(154)
11.7%
(115)
8.5%
(84)
7.3%
(72)
LDL-C not at goal
(
≥
1.8 /
≥
2.5 /
≥
3.0 mmol/l)
Elevated TG
(
≥
1.7 mmol/l)
Low HDL-C
(
<
1.0 male /
<
1.2 female mmol/l)
Fig. 3. Distribution of no, single and multiple combined
lipid abnormalities for the total study population. TG,
triglycerides; HDL-C, high-density lipoprotein choles-
terol; LDL-C, low-density lipoprotein cholesterol; propor-
tions add up to 99.9% because of rounding; thresholds
for LDL-C are based on the ESC guidelines (2011):
SCORE risk 1–4%: LDL-C
≥
3.0 mmol/l; patients with
SCORE risk 5–9%: LDL-C
≥
2.5 mmol/l; patients with CVD,
DM, and/or SCORE risk
≥
10%: LDL-C
≥
1.8 mmol/l.
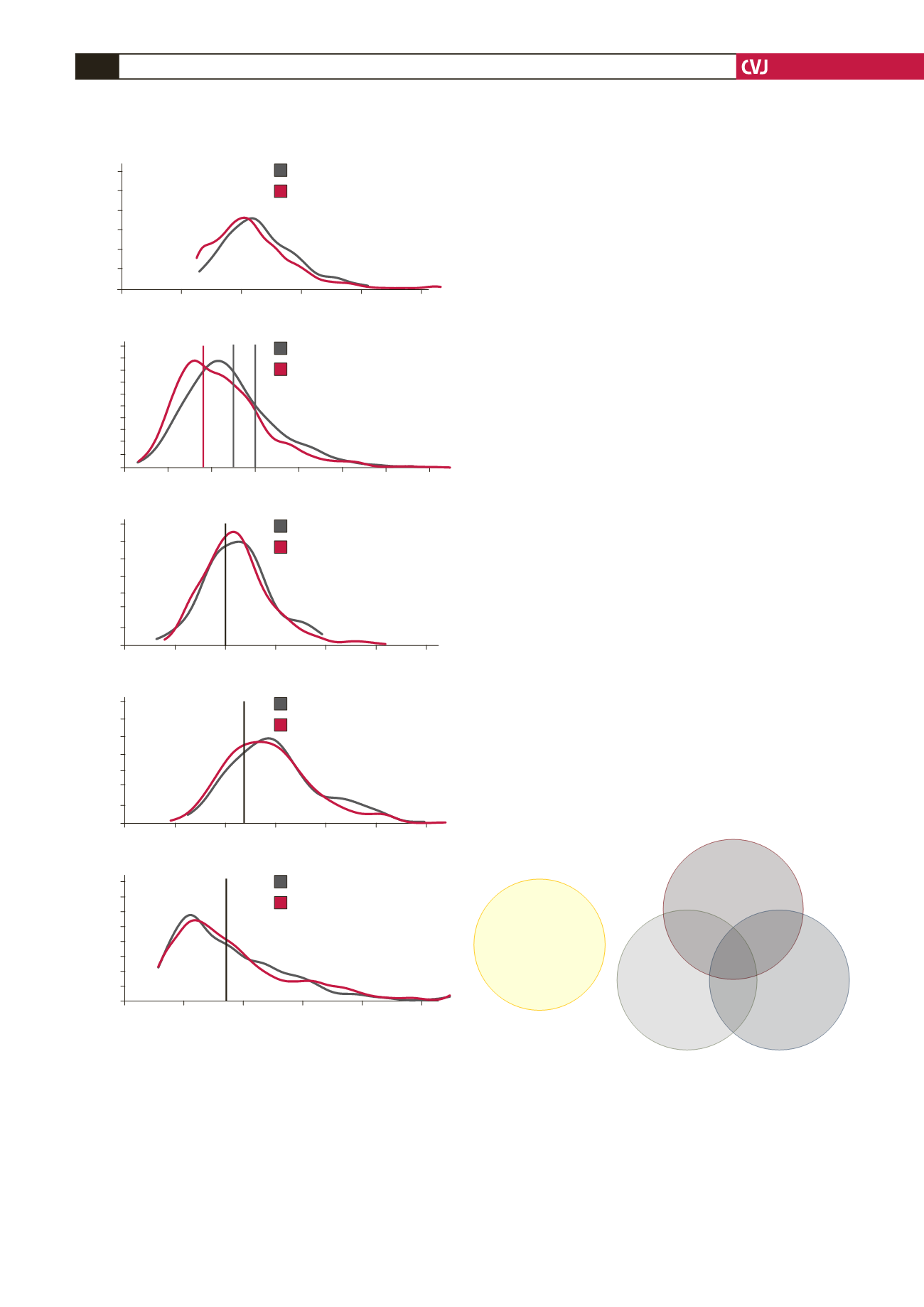
Fig. 2. Kernel density curves of lipids. Density curves
were unimodal and positively skewed throughout. The
data indicate that the very high-risk group (B) showed
slightly lower overall LDL-C levels than non-very high-
risk patients. Moreover, we observed that women (D)
maintained higher overall HDL-C levels than men (C)
in both the very-high and non-very high-risk groups,
while triglyceride levels were similar between the two
risk groups (E). Density curves for total cholesterol
were mostly overlapping (A). Vertical lines mark the cut-
off point of ESC guidelines (2011); LDL-C, low-density
lipoprotein cholesterol; HDL-C, high-density lipoprotein
cholesterol; TG, triglycerides.
0.6
0.5
0.4
0.3
0.2
0.1
0
0
2
4
6
8
10
Total cholesterol (mmol/l)
Density
Non-very high-risk patients
Very high-risk patients
A
0.5
0.45
0.4
0.35
0.3
0.25
0.2
0.15
0.1
0.05
0
0
1
2
3
4
5
6
7
LDL-C (mmol/l)
Density
Non-very high-risk patients
Very high-risk patients
B
1.4
1.2
1
0.8
0.6
0.4
0.2
0
0
0.5
1
1.5
2
2.5
3
HDL-C (mmol/l) in men
Density
Non-very high-risk patients
Very high-risk patients
C
1.4
1.2
1
0.8
0.6
0.4
0.2
0
0
0.5
1
1.5
2
2.5
3
HDL-C (mmol/l) in women
Density
Non-very high-risk patients
Very high-risk patients
D
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0
1
2
3
4
5
TG (mmol/l) in men
Density
Non-very high-risk patients
Very high-risk patients
E