
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 5, September/October 2014
e10
AFRICA
mainly in the apical, lateral and anterior walls, and mid-septal
portions of the left ventricle (Fig. 1A, B, C). There were no
co-existing cardiac abnormalities detected.
Non-compacted areas of the left ventricle were easily
distinguished from healthy segments by magnetic resonance
imaging (Fig. 2A). Coronary angiography revealed normal
coronary anatomy. The inter-trabecular recesses in the LV
wall were demonstrated by ventriculography (Fig. 2B). In
addition, sustained ventricular tachycardia was induced during
electrophysiological study (Fig. 3). Medical cardioversion with
1 200 mg iv amiodarone was administered to convert the
arrhythmia to sinus rhythm to haemodynamically stabilise the
patient.
The patient was put on amiodarone and anticoagulant
therapy in addition to optimal heart failure treatment consisting
of metoprolol 50 mg, ramipril 2.5 mg, furosemide 40 mg and
spironolactone 25 mg po qd. After implantable cardioverter-
defibrillator (ICD) implantation, the patient was discharged
and advised to continue the treatment. We also recommended
echocardiographic evaluation of her first-degree relatives,
considering the familial association of INVM.
Discussion
The incidence of non-compaction cardiomyopathy is about
0.05% in adults. Non-compaction of the LV myocardium is the
result of an arrest in compaction of myocardial fibres during
embryogenesis. It is most frequently observed in the left ventricle
but the right ventricle may also be affected. The disorder is
diagnosed by two-dimensional echocardiography.
3
Computed
tomography and magnetic resonance imaging (MRI) have
been reported as useful diagnostic tools in INVM; they may
be of value, especially in patients with poor image quality on
echocardiography.
5
The four previously established morphological criteria
for echocardiographic diagnosis of INVM is as follows; (1)
appearance of at least four prominent trabeculations and deep
inter-trabecular recesses; (2) appearance of blood flow from the
ventricular cavity into the inter-trabecular recesses as visualised
by colour Doppler imaging; (3) the segments of non-compacted
myocardium mainly involve the apex and the inferior mid-
and lateral mid-LV wall and typically show a two-layered
structure with an end-systolic ratio greater than two between
the non-compacted sub-endocardial layer and the compacted
sub-epicardial layer; and (4) absence of co-existing cardiac
abnormalities.
6
In a study by Jenni
et al
., the prevalence of non-compacted
cardiomyopathy was determined at 0.04% in five years.
7
Ventricular non-compaction was an isolated finding in 74% of
the cases and non-compacted ventricular myocardium involving
only the left ventricle was 62%. While 77% of patients were in
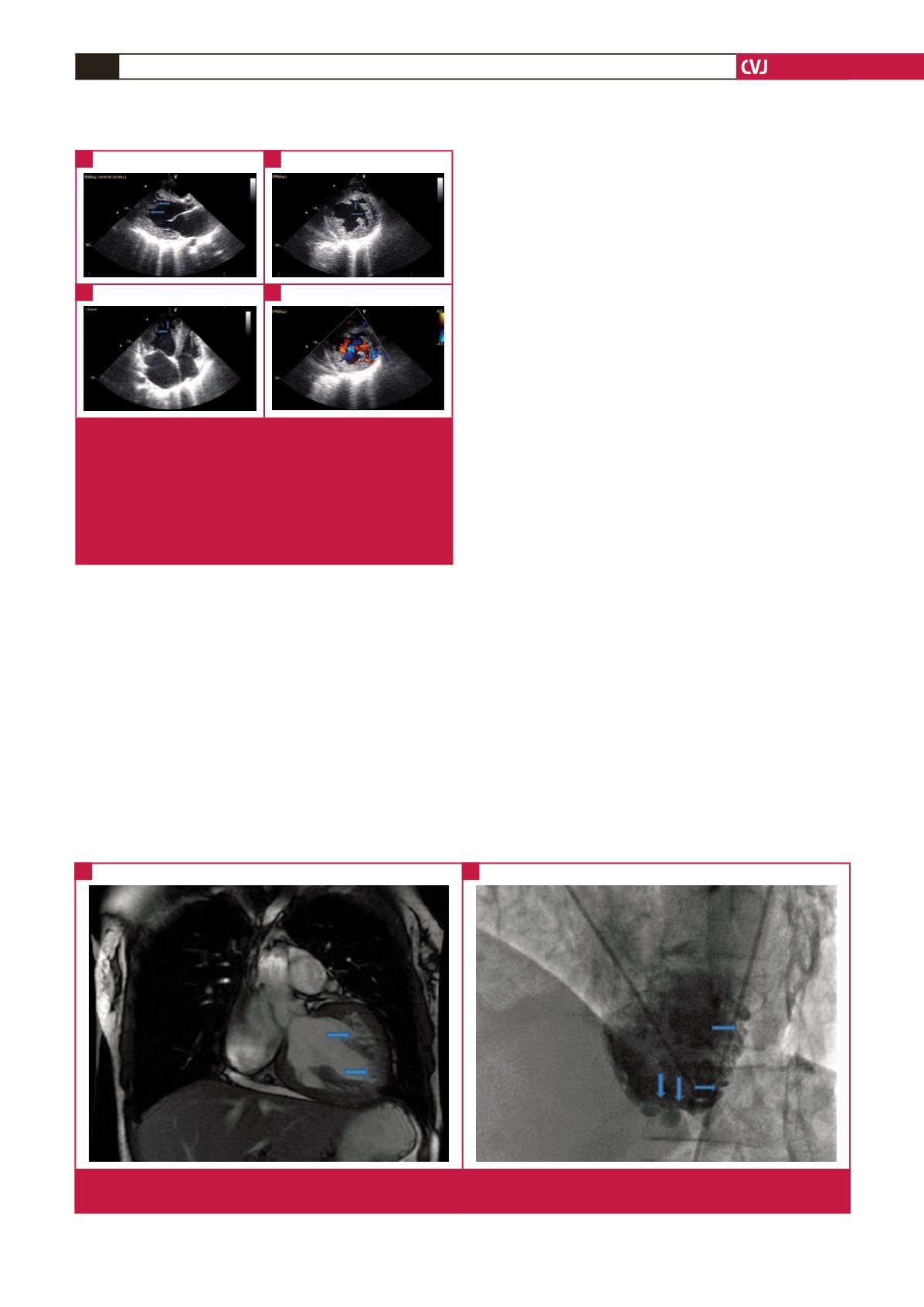
Fig. 1.
Transthoracic two-dimensional parasternal long-axis
(A), parasternal short-axis (B), and apical four-chamber
(C) images show isolated non-compaction of the left
ventricle with multiple trabeculae and inter-trabecular
recesses in the lateral, apical, anterior and mid-septal
areas. Appearance of blood flow from the ventricular
cavity to these deep trabeculae was detected by colour
Doppler imaging (D).
A
C
B
D
Fig. 2.
(A) Multiple deep trabeculae and inter-trabecular recesses of the left ventricle can also be demonstrated by MRI. (B) Left
ventriculogram of the patient showing inter-trabecular recesses, especially in the left ventricular apical and lateral wall.
A
B



















