CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 6, November/December 2014
266
AFRICA
and echocardiographic parameters, diagnosis, comments and
outcome.
Statistical analysis
Data were computed and analysed using Epi version 6.02. For
the purpose of this report, only the echo findings were included
in the analysis.
Results
During the period of four years, 23 124 children presented at the
Paediatric Department of the two centres. Of these, 440 children
were referred for echocardiographic evaluation. Only 356 (81%)
had echo done, out of whom 24 were found to have structurally
normal hearts. Therefore 332 patients with cardiac anomalies
were analysed. Prevalence of CHD in this hospital-based study
was 14.4 per 1 000 children.
Of those analysed, there were 174 males (52.4%) and 158
females (47.6%) in a ratio of 1:1. The ages ranged from 0.25
to 180 months with a mean of 26.1 months. Thirty (9%) of the
children were aged one month or less, 62% were between one
month and one year, 24.4% between one and five years, and
13.7% above five years of age.
The commonest indications for an echo were murmur in
36% (of which 6% were incidental murmurs), fast breathing in
19.8%, failure to thrive in 11% and cyanosis in 9.9%. Others
included features of dysmorphism and easy fatigability (Table 1).
Thirty-six (11%) of the patients had features suggestive of Down
syndrome (DS), while one patient had dysmorphism suggestive
of William’s syndrome.
9
Of the 36 patients with DS, over 60%
had multiple cardiac defects, with ventricular septal defects
(VSD)/patent ductus arteriosus (PDA) and VSD/atrial septal
defect (ASD) accounting for 50%. Nine patients had congenital
Rubella
syndrome, with PDA accounting for over 50% of the
cardiac defects.
Two hundred and seventy-seven (83.4%) of the patients
had acyanotic CHD and 55 (16.6%) had cyanotic CHD. In the
acyanotic group, there were 149 males (53.8) and 128 females
(46.2%), with no statistically significant difference, while there
were 25 males (45.5%) and 30 females (54.5%) in the cyanotic
group.
In the acyanotic group, solitary VSDs accounted for 32.5% of
cases, solitary PDAs for 17.3% and solitary atrial septal defect
(ASD) for 8.3%. Atrio-ventricular canal defect (AVCD) was seen
in eight (2.9%) (Table 2). Congenital dilated cardiomyopathy was
seen in two patients, one of whom had lost two older siblings
in infancy with similar conditions. Of the two patients with
hypertrophic cardiomyopathy, one was a macrosomic infant
of a diabetic mother, who had spontaneous resolution of the
hypertrophy by the fourth month. The other was an infant of a
non-diabetic mother, who was managed in a peripheral hospital
and died after two months from recurrent heart failure.
In the cyanotic group, transposition of the great arteries
(TGA) was seen in 12 patients, and tetralogy of Fallot (TOF)
in 28 patients, two of whom had associated ASD (pentalogy of
Fallot). Truncus arteriosus was seen in three patients (Table 3).
Table 4 shows the number of children with multiple congenital
heart diseases.
Of the children studied, 24 (7.2%) have had successful
surgeries in India, one in Ghana, one in South Africa and
three in the United State of America. Two children with atrio-
ventricular septal defect and pulmonary hypertension, who
had Eisenmenger syndrome, went to India and were confirmed
inoperable after cardiac cathetherisation.
One hundred and thirty-three (40%) of these children have
had at least one hospital admission, and 10 (3%) have died.
Four died in hospital while the other six were confirmed dead by
telephone calls from parents. Of those who died in hospital, two
had tetralogy of Fallot with cerebrovascular accident and died
after partial exchange of blood for packed cell volume of 88 and
76%, respectively. The other two died of intractable heart failure.
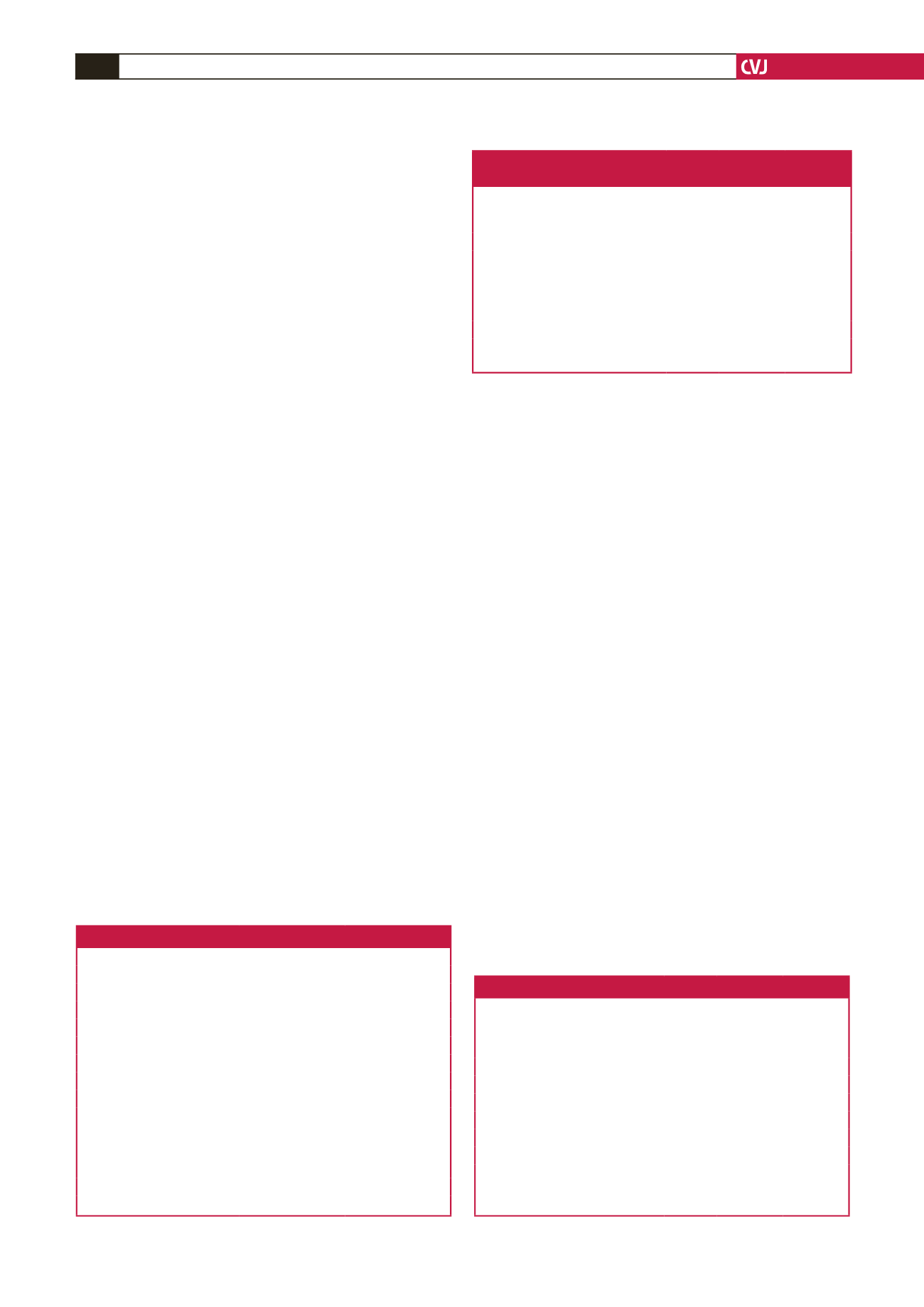
Table 1. Indications for echocardiography
Sign/symptom
Number of patients % of patients
Fast breathing
64
19.2
Failure to thrive
36
10.8
Murmur
83
25
Dysmorphism
36
10.8
Cyanosis
32
9.6
Recurrent pneumonia
13
3.9
Recurrent cough
16
4.8
Easy fatigability
23
6.9
Chest pain
6
1.8
Cardiomegaly on chest X-ray
6
1.8
Palpitation
5
1.5
Fainting attacks
6
1.8
Heart failure
21
6.33
Pre-term low birth weight
7
2.1
Table 2. Solitary acyanotic CHD types and frequency of
occurrence
Type of acyanotic CHD
No of
patients
% of acya-
notic CHD
(
n
= 277)
% of total
CHD
(
n
= 332)
Ventricular septal defect
90
32.5
27.1
Patent ductus arteriosus
48
17.3
14.5
Atrial septal defect
23
8.3
2.5
Pulmonary stenosis
3
1.1
0.9
Atrio-ventricular canal defect
8
2.9
2.4
Congenital dilated cardiomyopathy 2
3.6
0.6
Congenital hypertrophic cardio-
myopathy
2
3.6
0.6
Table 3. Cyanotic CHD types and frequency of occurrence
Type of cyanotic CHD
No of
patients
% of
cyanotic
CHD
(
n
= 55)
% of total
CHD
(
n
= 332)
Tetralogy of Fallot
28
50.9
8.4
Transposition of the great arteries
12
21.9
3.6
Tricuspid atresia
3
5.5
0.9
Truncus arteriosus
3
5.5
0.9
Double-outlet right ventricle
3
5.5
0.9
Ebstein’s anomaly
3
5.5
0.9
Hypoplastic left heart syndrome
2
3.6
0.6
Partial anomalous pulmonary
venous connection
1
1.8
0.3



















