
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 1, January/February 2015
AFRICA
27
in a continuous fashion with a 7-0 polypropylene suture. The
descending aorta was used for the inflow in all patients. When
the target vessel was identified posterolaterally, four stabilising
sutures were placed at each corner.
8
After arteriotomy, to achieve
a comfortable distal anastomosis, a fine vascular occlusion
clamp was used to stop bleeding and the distal anastomosis was
performed continuously with an 8-0 polypropylene suture. The
position and length of the graft was controlled meticulously to
protect it from kinking (Fig. 4).
9
Results
All operations were performed without CPB and electively via
thoracotomy. None required conversion to resternotomy or
institution of CPB. The average surgery time was 143.90
±
36.93
minutes. The number of anastamoses was 1.1875
±
0.39 per
patient (38/32). Average ICU stay was 21.3
±
4.41 hours with
5.08
±
1.88 hours of respiratory assist, and drainage was 497.65
±
291.43 ml. Average hospital stay was 5.06
±
2.74 days (Table 3).
The follow-up period was 56.17
±
39.2 months (1–152) post-
operatively. Twenty-two of 32 patients were alive and well, six
patients were lost in the follow-up period and four patients died.
There was no in-hospital mortality. All were discharged free of
angina. No peri-operative myocardial infarction was observed,
none of our patients required intra-aortic balloon pump (IABP)
and no renal failure occurred. One patient recovered with the
help of positive inotropic support. Atrial fibrillation developed
in one patient, deep-vein thrombosis in another, and infection
occurred in the thoracotomy incision scar of a third patient.
Unfortunately one patient underwent a revision because of
bleeding.
Discussion
Redo CABG presents challenges that initial CABG surgery
does not pose. Re-operative technique and the deteriorating
condition of these patients cause raised morbidity and mortality
rates of re-operated patients compared with the initial CABG
patients.
6
The most serious complications in isolated redo CABG
are massive haemorrhage, injury to patent LITA grafts, and
embolisation of the patent but very atherosclerotic ascending
aorta and old venous grafts due to median resternotomy and
extensive dissection of the heart.
10-12
Recurrent coronary artery patients who are candidates
for re-operation tend to be affected more negatively by the
deleterious effects of CPB because of their decreased capacity
for cardiac contractility.
6
Off-pump redo CABG revascularising
the Cx and its branches via a left posterolateral thoracotomy
in carefully selected patients presents dramatically improved
consequences as a result of avoiding median resternotomy and
CPB.
5,13,14
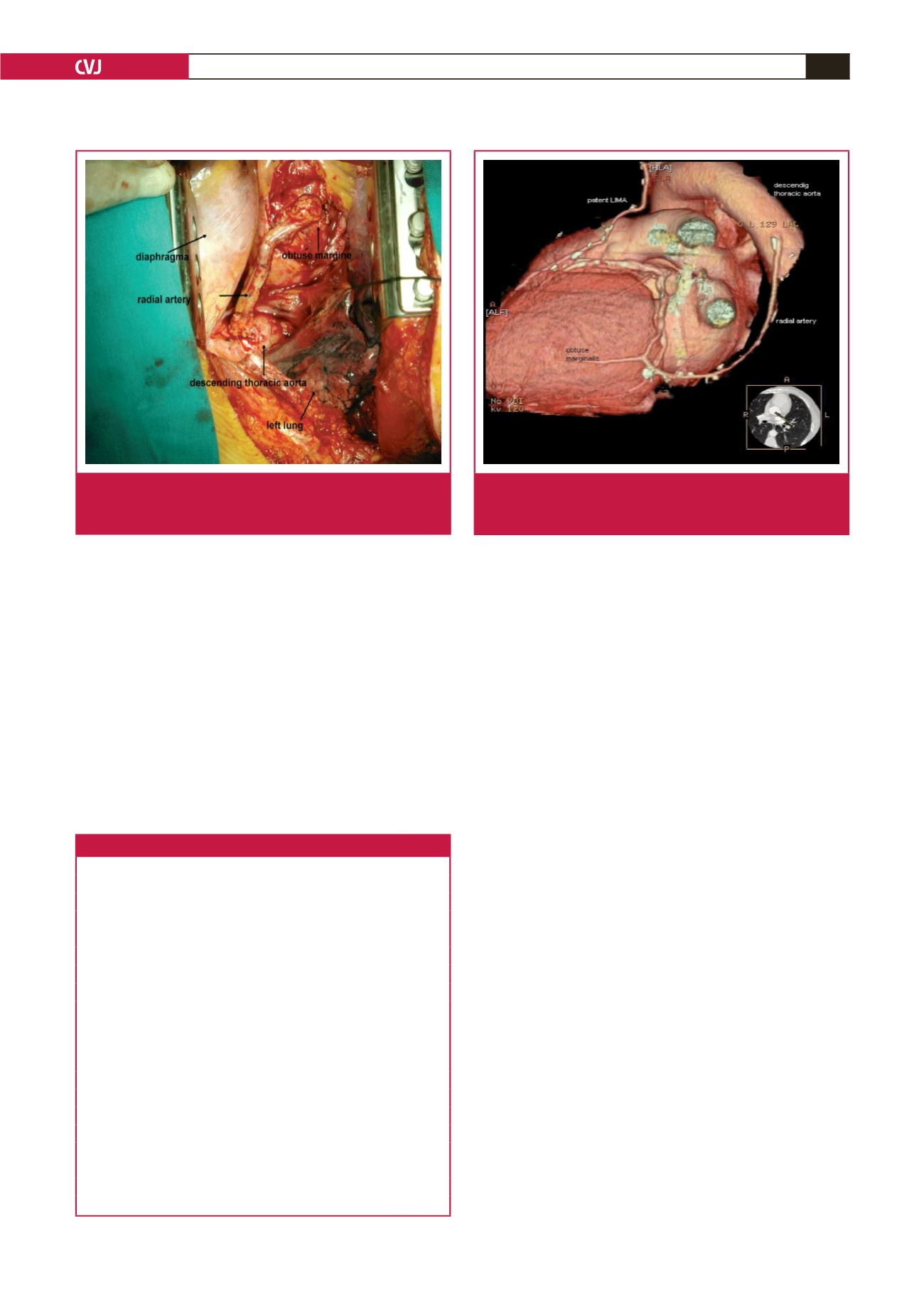
Fig. 3.
Operative view of redo off-pump CABG for the obtuse
marginalis branch of the Cx via a posterolateral thora-
cotomy.
Fig. 4.
The radial artery was anastomosed between the
descending thoracic aorta and obtuse marginalis
branch of the Cx without any kinking.
Table 3. Operative findings
Variables
Mean (n = 32) Min Max
Operation time (min)
143.90
±
36.93 90
270
Drainage (ml)
497.65
±
291.43 100 1550
Number of anastomoses
1.1875
±
0.39
1
2
Respiratory assist (h)
5.08
±
1.88
2
10
ICU stay (h)
21.3
±
4.41
14
36
Hospital stay (days)
5.06
±
2.74
4
18
Mortality
0
Early complications
Myocardial infarction
0
Use of IABP
0
(+) inotrope
1
Atrial fibrillation
1
Deep-vein thrombosis
1
Thoracotomy incision infection
1
Revision for bleeding
1
Follow up (months)
56.17
±
39.20
1
152
Alive and well
22
Lost to follow up
6
Dead
4



















